Sedation
BIS Monitor:
It is used to monitor the depth of sedation or anesthesia. BIS index is a practical processed EEG parameter that measures the direct effects of sedatives on brain. Used mainly in paralyzed patients who can’t communicate and hence, can’t use RASS scale.
The sensor on forehead sends raw EEG information to the BIS engine. This engine processes the EEG data according to an algorithm that combines select EEG features to produce a BIS index. This index is a number between 0 and 100 that is displayed on the monitor and reflects the patient's level of sedation. A patient who is awake and alert will have a BIS reading near 100, while one with no brain activity will have a reading of 0 and a flat EEG.
While BIS monitoring is reliable in a wide variety of patients and situations, in certain circumstances the BIS index may not accurately reflect a patient's level of sedation. The most frequent source of unreliable BIS readings is signal artifact from muscle activity, typically from the patient's face or forehead muscles. This muscle activity, measured as EMG in decibels, can be caused by pain, twitches, seizures, eye movement, or anything that results in increased muscle tone or movement. This activity can generate high-frequency signals that can contaminate the EEG and make the BIS index unreliable. For this reason, BIS monitors include an EMG bar graph. The higher the EMG, the greater the muscle activity, and therefore the less reliable the BIS index.
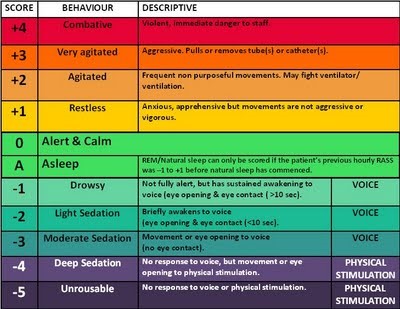
RASS Score:
Pitfalls of RASS/RAMSAY: sometimes can cause over sedation.
Analgesics
-
Morphine:
-
Onset of action: 5-10 mins
-
Duration of action: 2-4 hours.
-
Metabolism: It is metabolized in liver, has an active metabolite and excreted in urine. Dose needs to be adjusted if GFR<10
-
Dosage: 1-3mg bolus followed by 2-20mg/hr
-
Side effects: Hypotension, ileus, bradycardia, increased parasympathetic activity, hypoventilation. It also causes histamine release.
-
Dilaudid:
-
Onset of action: 5-10 mins
-
Duration of action: 2-4 hours.
-
Metabolism: It is metabolized in liver, has an active metabolite and excreted in urine. However, no dose adjustment needed for GFR<10
-
Dosage: 1-3mg bolus followed by 1-3mg/hr
-
Side effects: Hypotension
-
Fentanyl:
-
Onset of action: 1-2 mins
-
Duration of action: 30-60 mins.
-
Metabolism: It is metabolized in liver, but doesn’t have any active metabolite and excreted in urine. However, dose needs to be adjusted for GFR<10. It also accumulates in fat tissues and hence increased volume of distribution. Hence, there is increased risk of accumulation and delayed recovery.
-
Dosage: 1-3mcg/kg bolus followed by 25-700mcg/hr
-
Side effects: Hypotension
-
Tramadol: a synthetic opiate which is centrally acting. It is 10 times less potent than morphine.
-
Toradol:
-
Onset of action: 60 mins
-
Duration of action: 4-6 hours
-
Potency: 15mg of toradol is equal to 5 mg of morphine
-
MOA: NSAID’s
-
Side effects: it can inhibit platelet aggregation like all NSAID’s
Sedatives:
-
Ativan (Lorazepam):
-
Onset of action : 5-10 mins
-
Duration of action: 2-6 hours.
-
Metabolism: It is metabolized in liver and has no active metabolite. The inactive metabolite is excreted in kidney
-
Dosage: 2-8 mg/hr
-
Side effects: The drip is mixed in propylene glycol which can cause anion gap acidosis with osmolar gap. Also, prolonged sedation with BZD can accumulate and can cause prolonged delirium/confusion.
-
MOA: 20% receptor occupancy produces anxiolytic effect, 30-50% produces sedation and >60% produces hypnosis
-
Versed (Midazolam):
-
Onset of action : 2-5 mins
-
Duration of action: 1-3 hours. Can last longer in liver cirrhosis.
-
Metabolism: It is metabolized in liver to an active metabolite that is excreted in the kidney. (Note: In patients with AKI, versed may not be ideal choice since it has an active metabolite and gets excreted in urine. Use Ativan instead which has a predictable course in AKI. Ativan may infact be shorter acting than versed in AKI). Midazolam’s active metabolites are renally cleared and accumulate during kidney failure, prolonging sedation. Lorazepam is preferred for patients with impaired renal function; its metabolites are not active.
-
Dosage: 2-30 mg/hr
-
Propofol:
-
Onset of action : 1-2 mins
-
Duration of action: 45 mins.
-
Metabolism: It is metabolized in liver and has no active metabolite. Excreted by kidney.
-
Dosage: 1-3mg/kg bolus followed by 5-50mcg/kg/hr. In a 50 kg, it is usually 25-250mcg/hr. Doses as high as 200mcg/kg/hr is used for anesthesia.
-
Each ml of propofol has roughly 1 k.Cal because of lipid emulsion.
-
Side effects: Hyper-phosphatemia, hypotension and propofol infusion syndrome (Abrupt onset of heart failure, bradycardia, high CPK, hyperkalemia, elevated triglycerides, pancreatitis from elevated triglycerides, and lactic acidosis)
-
Uses: It decreases cerebral oxygen consumption and hence, it’s blood flow. So, it can be beneficial is patients with elevated ICP. Also causes less hypotension than other opiates.
-
Precautions: generally delivered from central line to prevent pain from infusion. Also, tubing and bottle has to be discarded every 12 hours to prevent bacterial infection.
-
Precedex (Dexmedetomidine):
-
Onset of action : 5-10 mins
-
Duration of action: 1-2 hours.
-
Metabolism: hepatic
-
Dosage: loading dose of 1mcg/kg infused over 10 mins followed by 0.3-0.7mcg/kg/hr. Mild hypertension with loading dose may be noted due to alpha stimulation. Continuous infusion may cause hypotension due to central sympatholysis causing vasodilation. Dose should be reduced in hepatic dysfunction.
-
Side effects: Bradycardia
-
MOA: It acts on alpha receptors rather than GABA receptors. In addition to sedation, Dexmedetomidine provides analgesic effects, a lack of respiratory depression, sympatholytic blunting of the stress response, preservation of neutrophil function (compared with the neutrophil- suppressing effect of GABA agonist medications), and may establish a more natural sleep-like state.
-
Uses: No effect on respiratory drive and hence, facilitates extubation.
-
Ketamine
-
Onset of action : 30 secs
-
Duration of action: 10 mins.
-
Dosage: Loading dose of 2mg/kg followed by 0.05-0.4 mg/kg/hr
-
Side effects: Sympathetic stimulation with increased heart rate, myocardial demand ischemia, increased ICP, bronchodilation
- Valium ( Diazepam)
-
Onset of action : 2-5 mins
-
Duration of action: 2-4 hours.
-
Metabolism: It is metabolized in liver and has active metabolite like versed.
-
Dosage: 1-3mg/hr
-
Side effects: Propylene glycol toxicity, dose dependent respiratory depression
-
Haldol
-
Onset of action : 10-20 mins
-
Duration of action: 2-6 hours.
-
Metabolism: It is metabolized in liver and has active metabolite like versed.
-
Dosage: 2-5mg loading dose followed by 10mg/hr which can be increased by 5mg/hr every 30 mins until agitation is resolved. Maximal doses are not defined and doses upto 200mg/day have been reported to be safe. Another method is to use 2mg initial dose and if no response, give another dose every 20 mins until agitation is resolved. However, the dose needs to be the double amount of previous dose each time.
-
Side effects: Hypotension, QT prolongation, anti-dopaminergic effects, Neuroleptic malignant syndrome ( hyperthermia, muscle rigidity and rhabdomyolysis), Torsades de pointes
-
Uses: mainly for acute delirium but no role in preventing delirium
- Seroquel/ Olanzapine: can be used to substitute haldol
Neuromuscular blockers
Neuromuscular blocking agents are used in the ICU setting:
-
To eliminate spontaneous breathing and promote mechanical ventilation (Rationale: High levels of PEEP, prolonged inspiratory time, inverse I: E ratios are uncomfortable for patients resulting in asynchrony between patient and ventilator thus the need for relaxation of respiratory muscles).
-
To transiently control excessive shivering and thereby decreasing oxygen consumption.
-
Decrease ICP
-
To reduce the metabolic demands of breathing
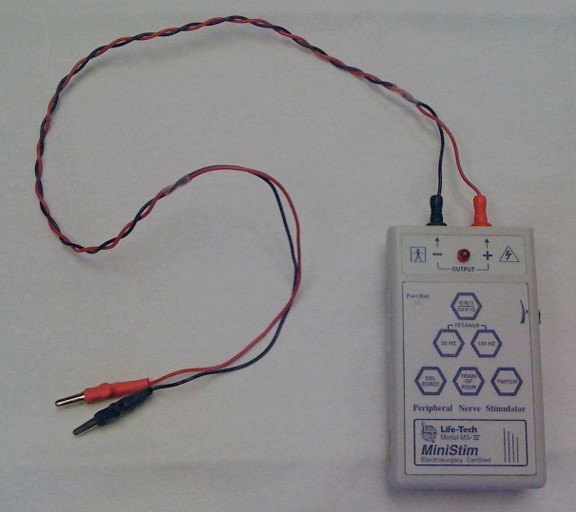
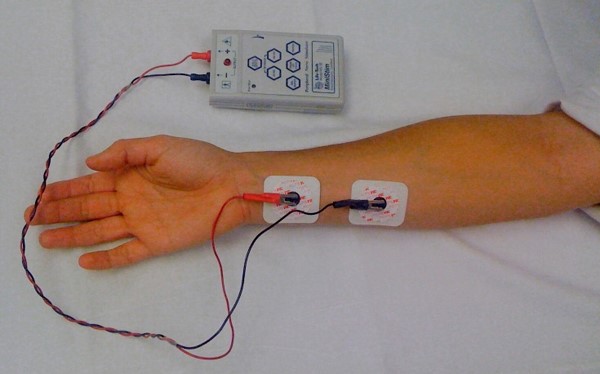
Train of Four test: Whenever a paralytic agent is used, the Train of Four test is used to measure the degree of neuromuscular blockade. By assessing the depth of neuromuscular blockade, peripheral nerve stimulation can ensure proper medication dosing and thus decrease the incidence of side effects. A peripheral nerve stimulator is used. Do a baseline measurement before paralytic agent is started to determine current necessary to obtain twitch. 20 mA may be enough for the patient. Complete and document until TOF to 2/4.
Instructions:
-
Attach 2 electrodes along the course of the ulnar nerve. (Place negative electrode on wrist in line with the smallest digit 1-2cm below skin crease and the positive electrode (red) 2-3cms proximal to the negative electrode. The Response is Adductor pollicis muscle – thumb adduction.
-
Connect the lead to the peripheral nerve stimulator by inserting the jacks into the Proximal (red) and Distal (black) output jacks. Connect the other end to the patient electrodes.
-
Turn on the peripheral nerve stimulator and select low amplitude, usually 10 or 20 mA to start. Increase the current in increments of 10 mA until 4 twitches are observed.
-
Press TOF once. It will deliver a train of four pulses where each is 0.5 seconds apart. Do NOT use the other buttons on the stimulator!
-
Count the number of twitches the patient had out of four (0/4, 1/4, 2/4, 3/4, 4/4.)
-
The response is measured as follows:
-
When 4 twitches are seen, 0-75% of the receptors are blocked.
-
When 3 twitches are seen, at least 75% of the receptors are blocked.
-
When 2 twitches are seen, 80% of the receptors are blocked.
-
When 1 twitch is seen, 90% of the receptors are blocked.
-
When no twitches are seen, 100% of receptors are blocked.
-
Adjust the medication as ordered. Goal is 1/4 to 2/4 twitches. Ideally, 4 twitches should occur two hours after discontinuation of neuromuscular blockers.
-
TOF should be assessed every 30 minutes x 4 or until ordered twitches achieved, then to q1h once goal TOF is achieved. If stable neuromuscular blockade is achieved, can do every 4 hrs.
Paralytics:
-
Succinyl Choline
-
Dose: Intial bolus of 1-1.5mg/kg
-
Onset of action: 30-60 seconds
-
Recovery: 4-6 mins
-
Side effects: Hyperkalemia
-
Contraindications: Rhabdomyolysis, AKI
-
MOA: Depolarizing neuromuscular blockers
-
Rocuronium
-
Dose: Intial bolus of 0.6-1.2mg/kg, followed by 0.5-0.7mg/kg/hr
-
Onset of action: 60-120 secs
-
Recovery: up to 30-60 mins
-
Contraindication: inability to oxygenate/ventilate
-
MOA: Non-Depolarizing neuromuscular blockers
-
Atracurium:
-
Dose: Intial bolus of 0.15mg/kg followed by 5-20 mcg/kg/hr
-
Onset of action: 2-3 mins
-
Recovery: 20-30 mins
-
Side effects: Hypotension
PEARLS:
-
For medical patients requiring >48 hrs of mechanical ventilation, sedation with propofol results in significantly fewer ventilator days compared with intermittent lorazepam, when sedatives are interrupted daily in both groups. (Crit Care Med 2006; 34:1326–1332)
-
There was no difference between dexmedetomidine and midazolam in the amount of time spent at targeted sedation level in mechanically ventilated ICU patients. Despite the similarity in sedation levels, dexmedetomidine-treated patients spent less time on the ventilator, experienced less delirium, and developed less tachycardia and hypertension. (JAMA. 2009;301(5):489-499)
-
Naloxone: antidote for opiate overdose. Start with 0.04mg and if no response in 2-3 mins, give 0.5mg and if no response in 2-3 mins, give 2mg and then 5mg 2-3 mins later. If still no response, possibly not opiate overdose. The response to Naloxone dose doesn’t correlate with degree of opiate overdose. Also, Naloxone is very short acting and wears off in 30-45mins and hence, patients may need prolonged therapy with Naloxone or intubation.
-
please make it print
Simple informative thank you for this.