Lung Ultrasound:
High frequencies are useful to look at the periphery of the lung with a high resolution as in looking for 'lung sliding' and other signs of pneumothorax, as well as studying lung comets. Lower frequencies help with the imaging of deep lung tissues as in looking at consolidation and pleural effusion. Hence a vascular probe is used for the assessment of pneumothorax, while the ultrasound probe is used for consolidation and pleural effusion.
Six regions, delineated by the anterior and posterior axillary lines should be systematically examined: upper and lower parts of the anterior, lateral and posterior chest wall.
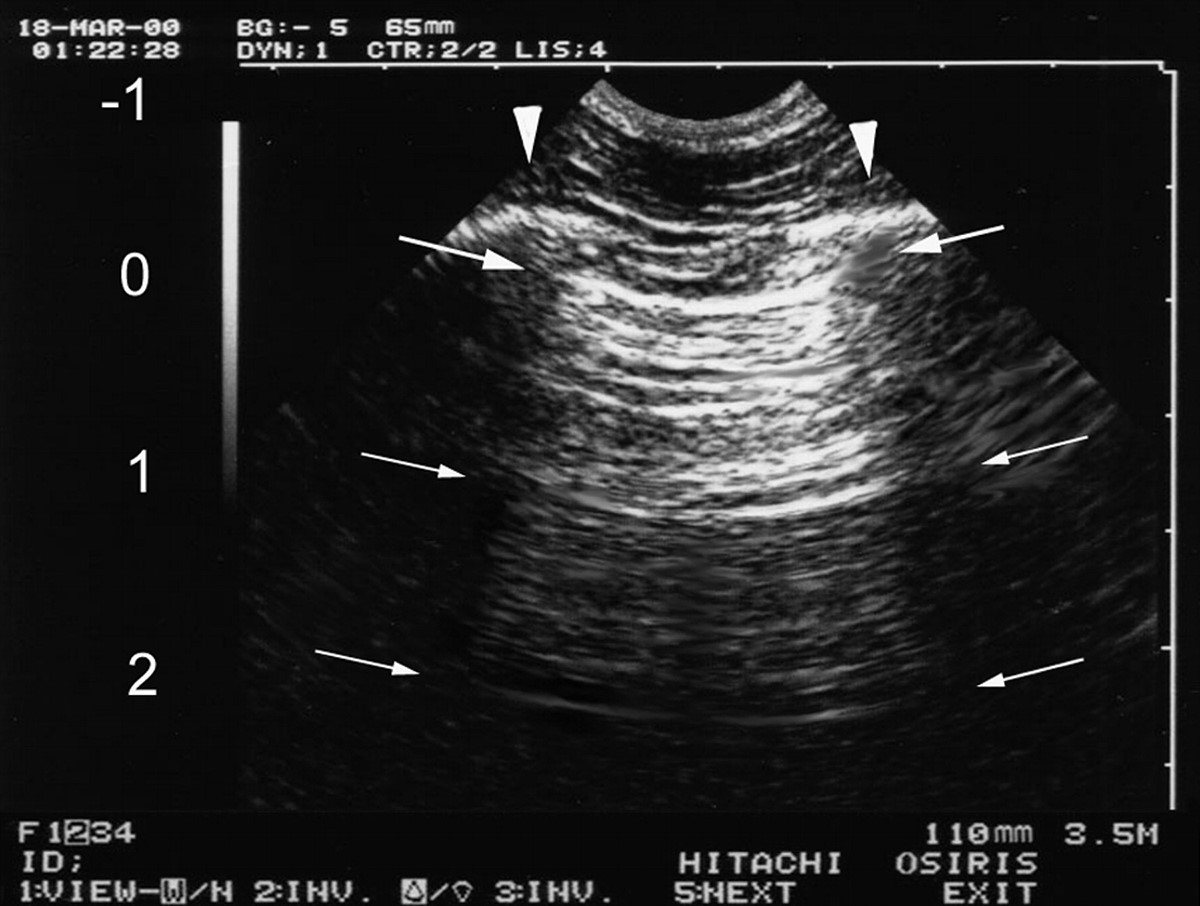
The probe is kept in the intercostal space with the marker pointing toward the head end of the patient. The ribs yield artefactual anechoic shadow images (black). In between the two ribs, there is a hyperechogenic line > 0.5cm deeper to the probe. This line is the interface between the soft tissues of the chest wall and the aerated lung the – "pleural" line. The air in normally aerated lungs stops progression of the ultrasound beam and hence the ultrasound "image" of the lung is composed of artifacts. These air artifacts arise from the pleural line.
A lines: Horizontal, regularly spaced hyperechogenic lines representing reverberations of the pleural line. These are motionless and are artifacts of repetition.
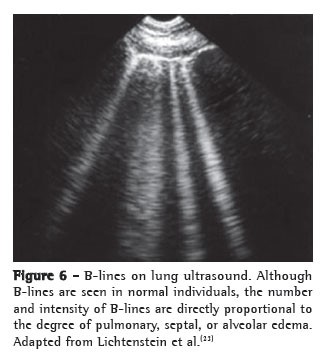
B lines: Vertical narrow based lines arising from the pleural line to the edge of the ultrasound screen. It extends to the edge of the screen and arises only from the pleural line. These are also called by the descriptive term "comet tail artifacts". When several B lines are visible, the term used is "lung rockets".
Z Lines: short, broad, ill defined, vertical comet tail artifacts arising from the pleural line but not reaching the distal edge of the screen are not B lines. These are called Z lines and are found in normal persons as well as in those with pneumothorax. They are less echogenic than the pleural line, usually taper off at after 2-4 cms, do not erase A lines and do not move with lung sliding.
Lung sliding sign:
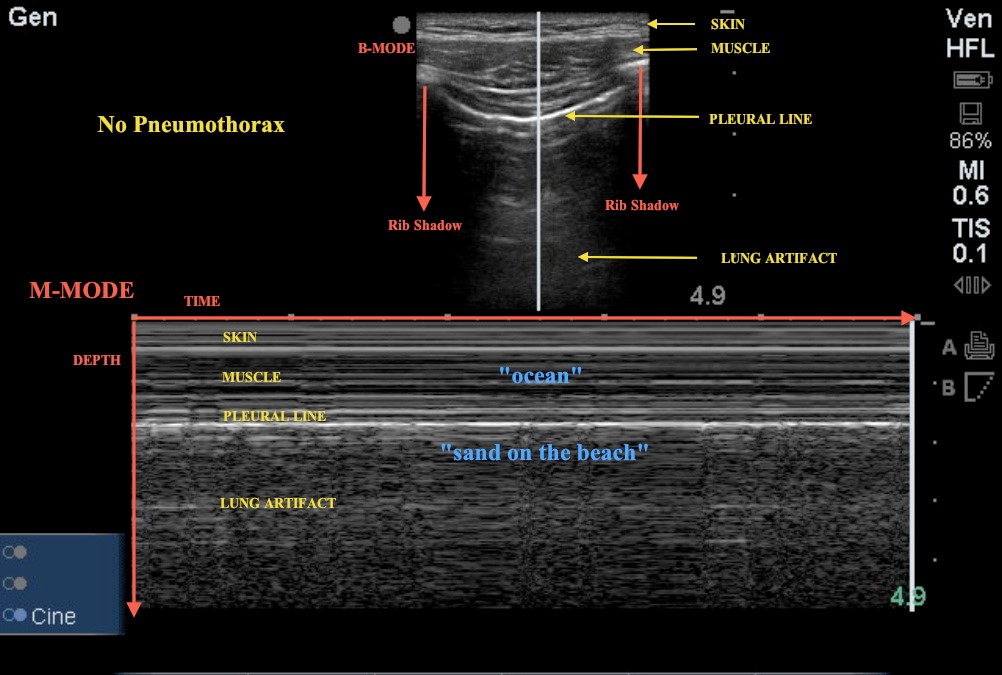
The pleural line "slides" (to and fro movement) with respiration. The movement is distinctive as the surrounding chest wall structures are still or move in an opposite direction to the lung. This is pleural / lung sliding. The sliding movement seen sonographically is the lung which moves on respiration.
The image best seen in an M mode as the superficial parietal layers are motionless and have a horizontal pattern of lines while the area deep to the pleural line appears "granular" as the motion of the pleural line is reflected all over this area. This is also known as the "seashore sign"
Pneumothorax
In the supine patient, a free pneumothorax usually collects in the anterior and non dependent area.
Absence of lung sliding: This is a sign of pneumothorax. If lung sliding is present, pneumothorax can be ruled out. However, loculated posterior, mediastinal and apical pneumothoracies can be missed. For a complete examination, the probe must be placed along the anterior, lateral and posterior intercostals spaces and observation must include a whole respiratory cycle at each point. In an M mode, this will show absence of the normal granular pattern deep to the pleural line – the whole picture will show a number of horizontal lines called as stratosphere sign.
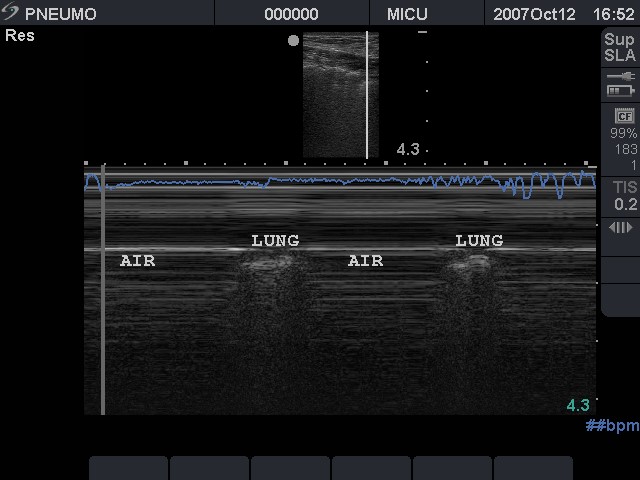
Horizontal lines have intermittently replaced the granular appearance of lung parenchyma suggesting a pneumothorax
Absence of B-lines: Although this is not specific for pneumothorax, the presence of B-lines rules out a pneumothorax. B-lines with absent lung sliding may be seen in lower lobe consolidations. Absent B-lines with lung sliding present may be seen in emphysema or hyperinflated lung states.
The lung point: Since the air in the pleural space moves anterior and the lung collapses to a dependent position posteriorly, there is a point, usually in the lateral regions where the lung and air may be visualized in the same view. On moving from anterior to lateral, a pneumothorax pattern gives way to a fleeting appearance of lung pattern in a particular location of the chest wall.
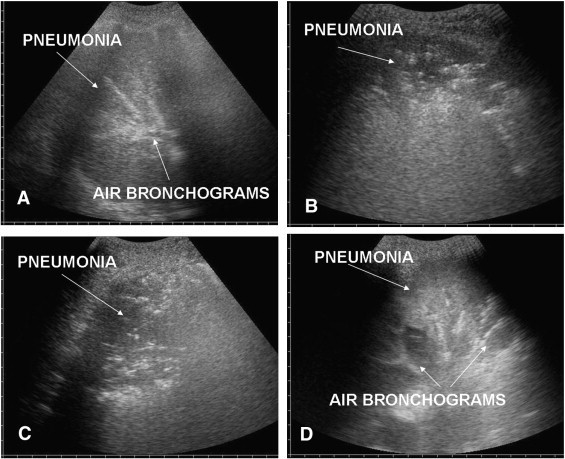
Pneumonia:
Within the consolidation, hyperechoic punctiform images can be seen corresponding to air in the bronchi – a so called ultrasound air bronchogram. These air bubbles can be seen to move in the bronchi during respiration.
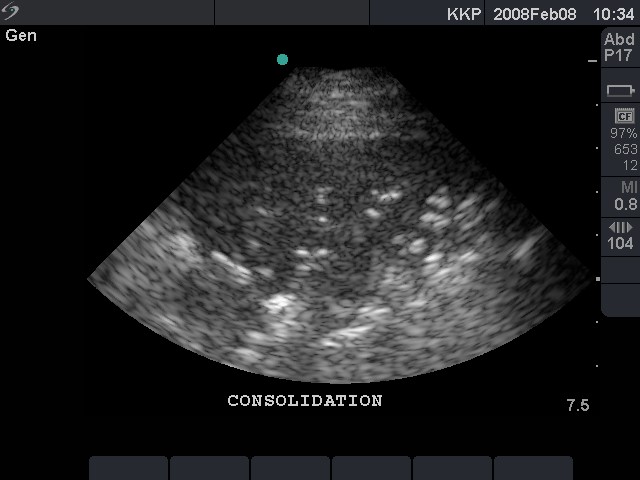
Lung hepatization:
Alveolar Interstitial syndrome:
A standard ultrasound probe in high resolution mode is used for this. It has been shown that multiple B-lines 7mm apart are caused by thickened interlobular septa representing interstitial edema, whereas B-lines 3mm or less apart are caused by ground glass areas characterizing alveolar edema
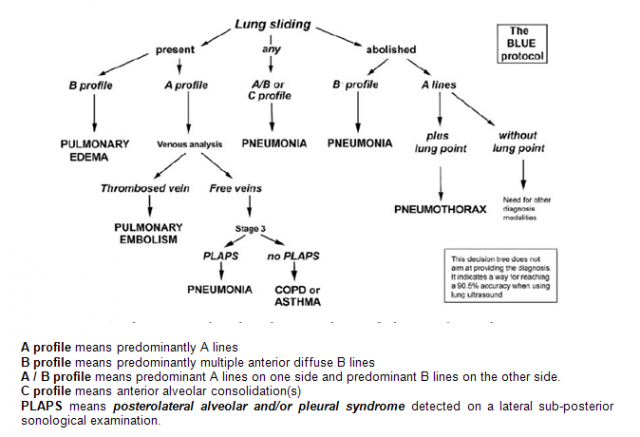
Blue Protocol:
Briefly, the B profile (anterior interstitial syndrome with lung sliding) indicated pulmonary edema. The B’profile (lung sliding abolished) indicated pneumonia.
The A/B profile (asymmetric anterior interstitial syndrome) and the C profile (anterior consolidation) indicated pneumonia, as did the A profile plus PLAPS. The A profile plus venous thrombosis indicated pulmonary embolism. A normal profile indicated COPD/asthma.
PLAPS (Posterolateral alveolar and/or pleural syndrome): Plaps point is the posterior continuation of blue point.
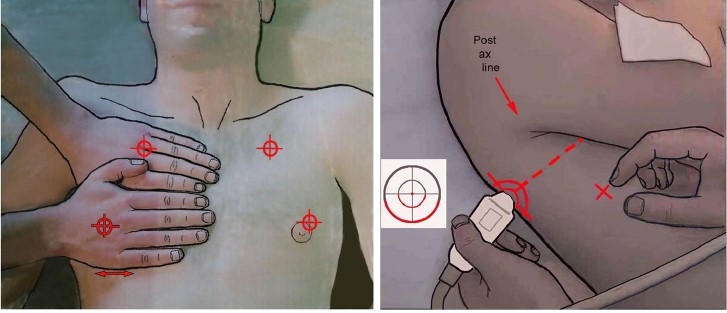
Two hands placed this way (size equivalent to the patient’s hands, upper hand touching the clavicle, thumbs excluded) correspond to the location of the lung, and allow three standardized points to be defined. The upper-BLUE-point is at the middle of the upper hand. The lower-BLUE-point is at the middle of the lower palm. The PLAPS-point is defined by the intersection of: a horizontal line at the level of the lower BLUE-point; a vertical line at the posterior axillary line.
Check for
-
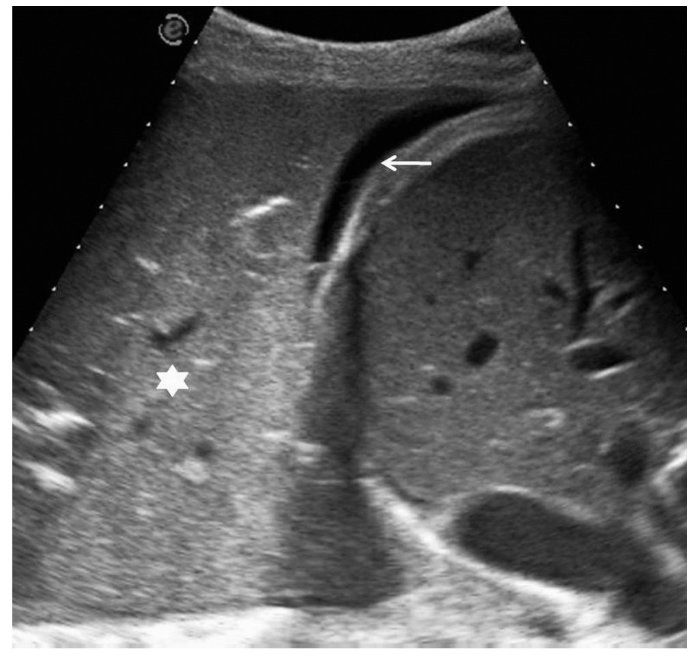
Pleural Effusion (hypoechoic region)
-
Consolidation (lung with Ultrasound appearance of liver without the sinusoids)
PEARLS:
-
Pleural effusions: Interpleural distance i.e. depth of at least 15mm, with effusion visible at the adjacent superior and inferior intercostal spaces is necessary in order to perform a safe pleural tap.
-
 Ref:
Ref:
Appreciating the time and energy you put into your site and detailed information you provide.
It’s awesome to come across a blog every once in a while that isn’t the same outdated rehashed information. Great read!
I’ve bookmarked your site and I’m including your RSS feeds to my Google account.