Airway Pressure Release Ventilation
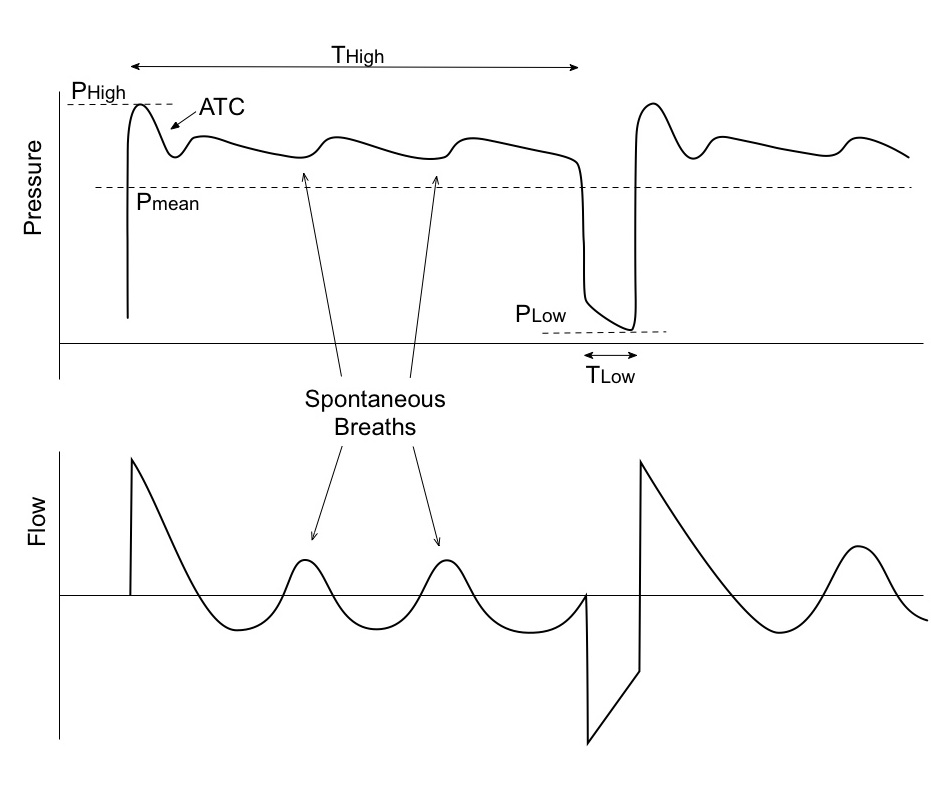
Airway pressure release ventilation (APRV) mode of mechanical ventilation is an elevated CPAP level with timed pressure releases. This short release for brief periods along with spontaneous breathing promotes CO2 elimination. Release time is short enough to prevent peak expiratory flow from returning to a zero baseline. The other advantage of APRV is that it uses lower peak and mean airway pressures to provide oxygenation.
A baseline high is set first. Mandatory breaths are achieved by releasing the high baseline pressures to Plow, which allows the lungs to deflate and then quickly resuming the pressure before the alveoli could collapse. This mode allows for spontaneous breathing. These breaths can be unsupported, pressure supported, or supported by automatic tube compensation. They key is a dynamic expiratory valve in the circuit which allows spontaneous breathing at high lung volumes. While any patient can be adequately supported using APRV, it is generally used for patients who require recruitment of alveoli to maintain oxygenation, such as in ARDS.
APRV should be seen as full tidal volume ventilation – the patient is ventilated on the expiratory limb of the volume pressure curve. Several "rules" are involved in APRV:
-
The expiratory time (Tlow) is the key variable – it should be short enough to prevent derecruitment and long enough to obtain a suitable tidal volume. The expiratory time is set between 0.4 to 0.6 seconds – the tidal volume is your target (between 4 and 6ml/kg). If the tidal volume is inadequate, the expiratory time is lengthened; if it is too high (>6ml/kg), the expiratory time is shortened.
-
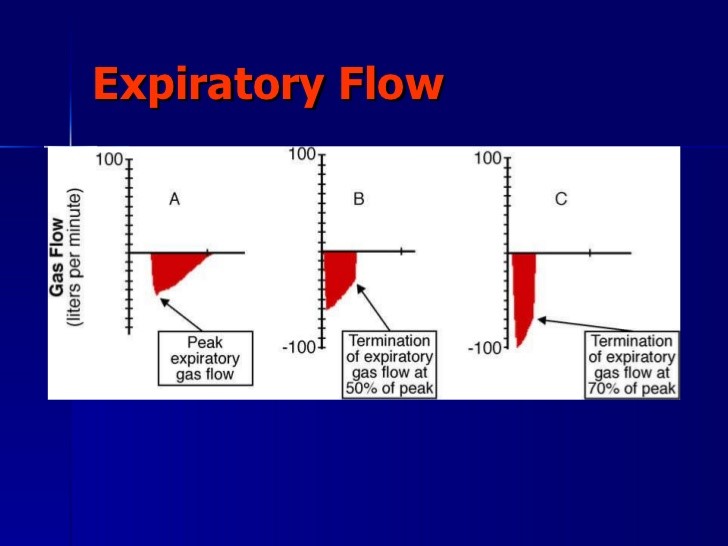
Generally, the TLow can be as short as 0.3 seconds (closer to 75% of PEFR) in restrictive disease and as long as 1.5 seconds (closer to 25% of the PEFR) in obstructive states. Set Tlow such that expiratory flow from patient ends at 40-60% of peak expiratory flow. This is to prevent complete collapse of alveoli. It should be short enough to prevent derecruitment but long enough to allow alveolar ventilation.
-
Tlow is generally set at one time constant (compliance x resistance). Time constant is the time it takes to empty 63% of lung volume.
-
Phigh is the upper CPAP level and analogous to mean airway pressure. Hence, it aids in oxygenation.
-
The high CPAP (PEEP) level is set at the mean airway pressure level from the previous mode (pressure control, volume control etc). A good starting level would be 28 cmH2O or previous plateau pressure. Higher transalveolar pressures recruit additional alveoli, but, try to keep PHigh below 30 cmH2O.
-
Low PEEP is set at 0cmH2O to optimize expiratory flow. The large pressure drop allows for tidal ventilation in very short expiratory times.
-
The difference between Phigh and Plow determines flow out of lungs and volume exchange, thereby affecting Tv and PCO2.
-
The inspiratory time is set at 4-6 seconds (the respiratory rate should be 8 to 12 breaths per minute – never more). The target is oxygenation.
-
Automatic tube compensation (ATC) should be on if spontaneously breathing.
-
The open exhalation valve allows for spontaneous breathing during THigh.
-
Neuromuscular blockade should be avoided: the patient should be allowed to breathe spontaneously (this is beneficial). The breaths can be supported with pressure support – but the plateau pressure should not exceed 30cmH2O.
-
There are two different ways to wean patients from APRV. If lung mechanics rapidly return to normal, the patient should be weaned to pressure support. If ARDS is prolonged, then the high CPAP level is gradually weaned down to 10cmH2O, and then the patient is converted to a standard vent wean.
-
If High CPAP <30cmH2O, the spontaneous breaths can be supported with pressure support, but plateau pressure should not exceed 30cmH2O.
-
If the patient remains severely hypoxemic, lengthen the inspiratory time further
-
If the hypoxemia improves significantly, reduce the inspiratory time to increase the respiratory rate and reduce hypercapnia.
-
Allow permissive hypercapnia. If pH <7.2, correct metabolic component (base deficit due to renal or hyperchloremic acidosis ) with sodium acetate (Na 140mmol/L) drip and, if PCO2 > 60mmHg start THAM
-
If hypoxemia worsens further consider Prone positioning or neuromuscular blockade.
-
Bi-level ventilation is the same as APRV but uses pressure support during spontaneous ventilation.
APRV should help rest the inspiratory muscles and utilize the diaphragm. Once the initial settings are applied, look for anterior chest muscles to be used much less and the diaphragm to be doing the majority of the work. The patient should be breathing more comfortably as recruitment occurs.
Making Adjustments to the APRV Settings
Oxygenation Options
-
When possible wean FiO2 to <50% for a SpO2 >90% or a PaO2 >60.
-
To improve oxygenation via higher PMean:
-
Increase PHigh in increments of 2 cmH2O.
-
Decrease TLow to be closer to 75% PEFR.
-
Increase THigh
-
Respiratory Acidosis
-
Increase PHigh (up to 40 cmH2O).
-
Increase THigh (if spontaneously breathing) in increments of 0.5 seconds up to 8 seconds. If PaCO2 increases with this change, it may reflect inadequate lung volume. If this is the case, try increasing PHigh to re-establish an adequate FRC.
-
Increase TLow to allow more time for alveolar emptying, but only if the expiratory flow of a release doesn’t drop below 25% of the PEFR.
-
If further increases in THigh fail to drop PaCO2, you may need to do the opposite: Decrease THigh to increase the rate of releases. This will decrease the PMean and oxygenation. This will then also increase PHigh to maintain the PMean. Maximize PHigh and release rate up to 30 (more like PC-Inverse Ratio ventilation).
-
If unable to manage the acidosis with APRV, the mode may be changed to PCV attempting to maintain the same rate and PMean.
Respiratory Alkalosis
-
Decrease PHigh (SpO2 may decrease).
-
Increase THigh to decrease the release state.
-
Turn ATC off if no spontaneous respirations.
Increased Respiratory Efforts
-
If the patient is consistently inhaling forcefully with accessory muscles, they may need alveolar recruitment. Options are:
-
Increase PHigh or THigh. This will elevate the PMean and encourage recruitment.
-
Decrease TLow only if you can maintain the flow during the release phase <75% of PEFR and the PaCO2 and pH are acceptable.
Forceful expirations
If the patient seems to be exhaling forcefully, over-inflation may be present. Try to decrease volumes or give more time for exhalation. Options are:
-
Decrease the PHigh in 1-2 cmH2O increments and increase THigh (to maintain the same PMean).
-
Increase the TLow. Allowing more time to exhale only if you can maintain the flow during the release phase >25% of PEFR.
-
CXR should be monitored for lung over-inflation.
APRV Weaning
When FiO2 is titrated below 50%, recruitment is maximized and the patient is breathing spontaneously, a continuous gradual wean can begin by:
-
Decreasing the PHigh by 1-2 cmH2O and increasing the THigh by 0.5 seconds for every 1 cmH2O drop in PHigh. This is referred to as the “drop and stretch”.
-
“Drop and stretch” should be done every two hours or more if tolerated. As you “drop and stretch” the PMean is gradually lowered, so you will need to monitor SpO2. Changing the CPAP or dropping PMean too quickly will possibly de-recruit alveoli.
-
Throughout the weaning process, the patient should be closely monitored for increasing work of breathing, tachypnea, or a drop in SpO2. If this occurs, return to the previous settings.
-
When the PHigh reaches 10 cmH2O and the THigh reaches 12-15 seconds, change the mode with CPAP of 10 or PEEP of 10 cmH2O and pressure support at 5-10 cmH2O. ATC should be off. Slowly wean CPAP was tolerated.
-
The patient should be spontaneously breathing throughout this process; therefore it is not necessary to do spontaneous breathing trials.
-
The main goal is to transition patient to CPAP with fewer releases ( by increasing THigh)
PEARLS:
-
Variables that affect oxygenation are mean airway pressure( depends on Phigh and Thigh) and FiO2
-
Variables that affect alveolar ventilation are Pressure gradient ( Phigh minus Plow), Tlow, airway pressure release frequency
-
Airway release during Plow provides for mandatory breaths and patient can have spontaneous breathing during any time of respiratory cycle.
-
APRV causes increased right ventricular afterload leading to worsening of pulmonary hypertension but decreases left ventricular afterload.
-
APRV increases venous return and may improve hemodynamics
-
APRV vs. BiPAP: both permit spontaneous breathing during both phases but there is no restriction of Tlow in BiPAP.
-
Time constant (t) is the time it takes to empty 63% of the lung volume; t = C x R (compliance x resistance). A rule of thumb is that complete emptying requires 4 x time constant (this is not achieved in APRV, hence auto PEEP results)
-
TOO
GOOD