Sodium and water balance
TBW (Males) = 60% of bodyweight
TBW (Females) = 50% of bodyweight
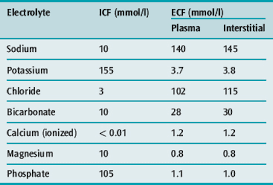
TBW = ECF (1/3rd) + ICF (2/3rd)
ECF = Intravascular (1/4th) + Extra vascular (3/4th)
Plasma Osmolarity = = 2[Na+] + [Glucose]/18 + [BUN]/2.8 + [Ethanol]/4.5
Loss of ECF volume can lead to a reduction in tissue perfusion. However, the ECF volume and tissue perfusion do not always change in the same direction. Two common examples are heart failure with edema and cirrhosis with ascites. In both disorders, the ECF volume is increased, but tissue perfusion is reduced due to a low cardiac output in most cases of heart failure and to vasodilation in cirrhosis. In both disorders, decreased tissue perfusion activates sodium-retaining hormones, which increase the extracellular volume but, due to the underlying disease, do not normalize tissue perfusion.
Changes in the intracellular fluid volume primarily occur when there are changes in plasma tonicity, resulting in water movement into or out of the cells. As described below, the intracellular and brain volumes usually increase with hyponatremia and decrease with hypernatremia.
I V Fluids
Dextrose
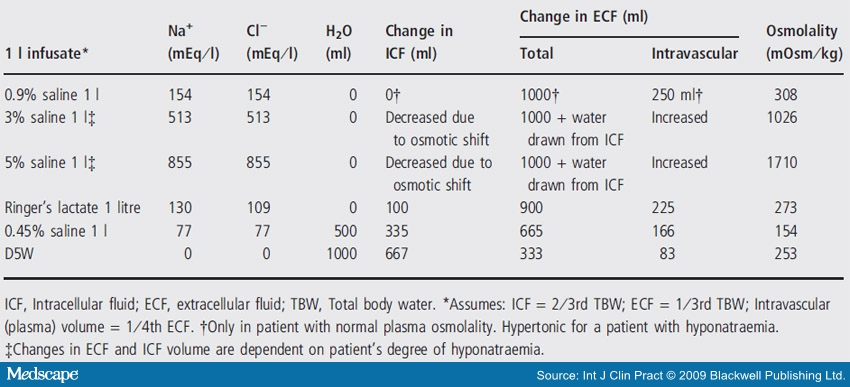
Dextrose solutions deliver water according to the natural distribution of body water. That means two thirds moves intracellularly, and only 8% or 80 mL of every liter remains in the intravascular space.
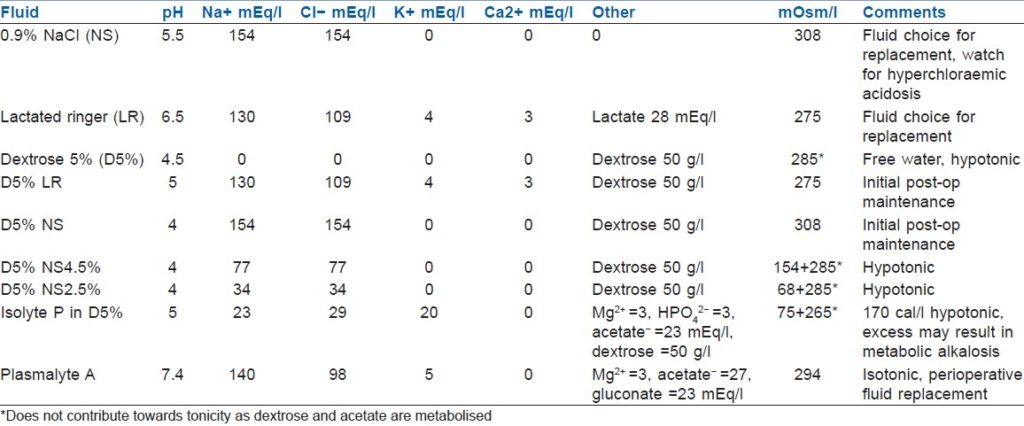
Crystalloids
Isotonic crystalloids (0.9 NS or LR) remain in the extracellular compartment and distribute between the interstitial and intravascular compartments at a 3:1 ratio. For every liter of normal saline administered 250 mL remain in the intravascular compartment. Hypotonic crystalloids (e.g. half normal saline) will distribute partly like dextrose solutions (across all three body compartments) and partly as crystalloids (Limited to the extracellular compartment).
Saline
Normal saline has a sodium concentration of 154 mmol/L, slightly hypertonic. The pH of normal saline is 5.5. This is the source of dilutional acidosis. When patients are given a large volume of normal saline they may develop a non-anion gap metabolic acidosis. This hyperchloremic acidosis is due to the acidic nature of normal saline. This is not seen with the other isotonic fluid, lactated ringers (pH 6.6).
Ringerʼs solution
Lactated Ringer is the crystalloid solution with an electrolyte composition very similar to plasma. Lactate is used as the source of alkali because bicarbonate has a poor shelf-life. Lactate is metabolized to glycogen which is ultimately converted to carbon dioxide and water by oxidative metabolism. Additionally, because of the calcium and potassium, it should not be used in patients with hypercalcemia or hyperkalemia.
Dehydration or Hypovolemia
Dehydration is often used as a synonym for volume depletion or hypovolemia. This is not technically correct and when discussing hyponatremia the distinction becomes important.
Dehydration means a loss of water in excess of sodium. Patients who become dehydrated become hypernatremic as total body sodium becomes diluted in less and less fluid.
Hypovolemia is loss of both water and sodium in roughly equal amounts. Hypovolemia can lead to hyponatremia in some cases but low serum sodium can be associated with low, normal or high volume status.
Sodium Balance:
The plasma sodium concentration is regulated by changes in water intake and excretion, not by changes in sodium balance. Hyponatremia is primarily due to the intake of water that cannot be excreted, hypernatremia is primarily due to the loss of water that has not been replaced, hypovolemia represents the loss of sodium and water, and edema is primarily due to sodium and water retention.
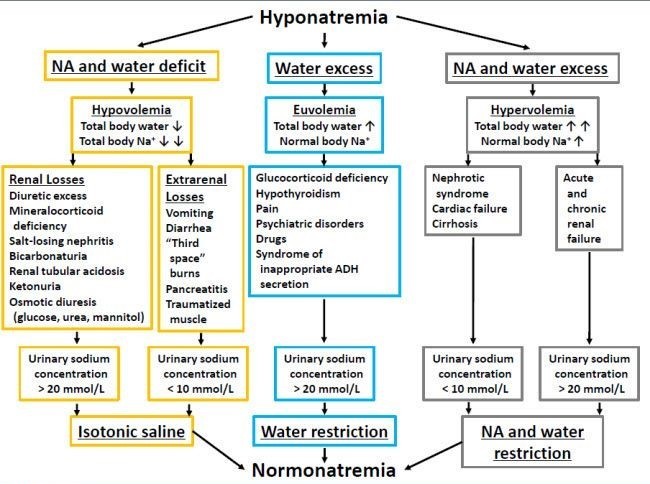
Hyponatremia
In virtually all patients, hyponatremia results from the intake (either oral or intravenous) and subsequent retention of water. A water load will, in normal individuals, be rapidly excreted as the dilutional fall in serum osmolality suppresses the release of antidiuretic hormone, thereby allowing excretion of the excess water in dilute urine.
In contrast to the response in normal individuals, patients who develop hyponatremia typically have impairment in renal water excretion, most often due to an inability to suppress ADH secretion. An uncommon exception occurs in patients with primary polydipsia who can become hyponatremic because they rapidly drink such large quantities of fluid that they overwhelm the excretory capacity of the kidney even though ADH release is appropriately suppressed.
In advanced renal failure, the minimum urine osmolality rises to as high as 200 to 250 mosmol/kg despite the appropriate suppression of ADH. The osmotic diuresis induced by increased solute excretion per functioning nephron is thought to be responsible for the inability to dilute the urine.
Reset Osmostat — In normal individuals, plasma antidiuretic hormone (ADH, arginine vasopressin) levels are very low when the plasma osmolality is below 280 mosmol/kg, thereby permitting excretion of ingested water, and increase progressively as the plasma osmolality rises above 280 mosmol/kg. Hyponatremia due to downward resetting of osmostat is one form of the SIADH. The presence of a reset osmostat should be suspected in any patient with apparent SIADH who has mild hyponatremia (usually between 125 and 135 meq/L) that is stable over many days despite variations in sodium and water intake.
High ADH can be due to physiological states as in high osmolarity, hypovolemia, hypotension (ADH is a potent vasoconstrictor), pain, anxiety, nausea and vomitings.
ADH release due to pathological states can be found in hypothyroidism, hypocortisolism, TB, sarcoidosis, CNS lesions like meningitis and cerebral abscess, SAH, drugs like TCA, Haldol and morphine, paraneoplastic syndromes with small cell cancer of lung, drugs that promote ADH action on kidney like aspirin, NSAID’s, caffeine and theophylline.
The normal response to hyponatremia (which is maintained in primary polydipsia) is to completely suppress ADH secretion, resulting in the excretion of a maximally dilute urine with an osmolality below 100 mosmol/kg and a specific gravity 1.003. Values above this level indicate an inability to normally excrete free water that is generally due to SIADH.
There are 4 criteria that must be met to make the diagnosis of SIADH:
1. Low serum sodium and low serum osmolality
2. Euvolemia
3. Inappropriately elevated urine osmolality (above 100 mosmol/kg and usually above 300 mosmol/kg)
4. Elevated urine sodium (usually >40meq/L).
Treatment:
Hypovolemic hyponatremia can be treated with administration of saline. In this setting, restoration of euvolemia will suppress the release of ADH (which has a half-life of only 15 to 20 minutes), thereby allowing rapid excretion of the excess water.
Fluid restriction — Fluid restriction to below the level of urine output is indicated for the treatment of symptomatic or severe hyponatremia in edematous states (such as heart failure and cirrhosis), the syndrome of inappropriate antidiuretic hormone secretion (SIADH), and advanced renal failure. Restriction to 50 to 60 percent of daily fluid requirements may be required to achieve the goal of inducing negative water balance. In general, fluid intake should be less than 800 mL/day.
An alternative or possible addition to fluid restriction and sodium chloride administration in patients with hyponatremia is the use of an ADH receptor antagonist like tolvaptan.
Hypertonic Saline administration:
Sodium deficit = Total body water (TBW) x (desired SNa – actual SNa)
Avoid overly rapid correction — Overly rapid correction of severe hyponatremia (serum sodium concentration almost always less than 120 meq/L and usually less than 115 meq/L) can lead to a severe and sometimes irreversible neurologic disorder called the osmotic demyelination syndrome. One group that is probably not at risk for this complication is patients with hyperacute hyponatremia that developed over a few hours due to a marked increase in water intake, as can occur in marathon runners, patients with primary polydipsia, and users of ecstasy. These patients have not had time for the brain adaptations that reduce the severity of brain swelling but also increase the risk of harm from rapid correction of the hyponatremia.
The goal of therapy is to raise the serum sodium concentration by 4 to 6 meq/L in a 24-hour period. Every effort should be made so that the increase in serum sodium is less than 9 meq/L in any 24-hour period and less than 18 in 48 hour period.
The clinical manifestations of ODS are typically delayed for two to six days after overly rapid elevation of the serum sodium concentration. The symptoms, which are often irreversible or only partially reversible, include dysarthria, dysphagia, paraparesis or quadriparesis, behavioral disturbances, lethargy, confusion, disorientation, obtundation, and coma, seizures and "locked in syndrome”.
Relowering the serum sodium if overly rapid correction has occurred —Relower the sodium in patients with an initial serum sodium concentration of 120meq/or less that has been present for more than two to three days (or with an unknown duration of hyponatremia) in whom the rate of correction has exceeded maximum recommended goals (less than 9 meq/L in any 24-hour period and less than 18 meq/L in any 48-hour period). It can be achieved with D5W, 6 mL/kg lean body weight, infused over two hours or Desmopressin, 2 micrograms intravenously or subcutaneously every six hours. The serum should be lowered at an average rate of approximately 1 meq/L per hour.
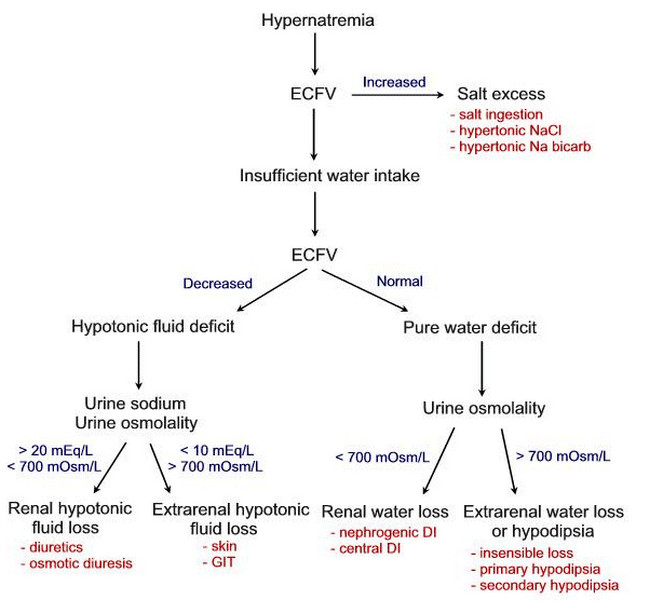
Hypernatremia
Hypernatremia causes an intense thirst and even with a complete lack of ADH (i.e. central diabetes insipidus) patients are able to maintain normal serum sodium by copious water drinking. This means that increased serum sodium is always due to an inability to drink water. Rarely patients may get hypernatremic from administration of excess sodium, usually after bicarbonate administration.
Hypernatremia causes cerebral desiccation. This result in shrinking of the brain and can tear the bridging vessels and result in intracranial hemorrhage.
A rise in the serum sodium concentration is associated with a rise in the plasma osmolality, which is a potent stimulus to both ADH release and thirst. A plasma osmolality above 295 mosmol/kg (which represents a serum sodium concentration above 145 to 147 meq/L) generally leads to sufficient ADH secretion to maximally stimulate urinary concentration. If the urine osmolality is less than the plasma osmolality (usually less than 300 mosmol/kg), then the patient has either central or nephrogenic diabetes insipidus (DI).
PEARLS:
-
Pure water can’t be excreted from kidneys as such and hence must be accompanied with some particles such as urea and electrolytes. The minimum urine osmolarity is 50m.mol/kg
-
Normal serum osmolarity is 280-300.
-
Pseudohyponatremia correction: for every 100 increase in sugars above 200, correct sodium by 1.6-2.1.
-
Pseudohyponatremia can also be due to hyperlipidemia and hyperprotenemia. However, the osmolarity is isotonic. Modern lab machines correct this and don’t give pseudohyponatremia. ( please note that lab machines do not correct for high glucose)
-
Normal saline bolus gets distributed only in extracellular space. Hence, 1 litre of NS bolus results in only 200-250ml that stays intravascular.
-
Average insensible loss is 8-12 ml/kg (60-75% resp + 25-40% skin). Daily insensible water losses are around 600ml and daily insensible water gain from oxidation of food is around 250ml.
-
Diarrheal fluid losses from large intestine are similar to 0.45NS in composition and fluid losses from pancreas/bile/small bowel are similar to 0.9NS in composition.
-
Hypertonic solutions are also considered plasma expanders as they act to increase the circulatory volume via movement of intracellular and interstitial water into the intravascular space.
-
The volume of distribution of bicarbonate is approximately that of total body water. However, if we infuse sodium bicarbonate, sodium remains in ecf and Bicarb is distributed like free water. This is in ideal scenario but in practice some of that Bicarb is metabolized into CO2 and H2O.
-
For each 100 ml of 3% hypertonic saline, the serum sodium concentration will increase by approximately 2 mmol/l.
-