Neutropenia is usually defined as an ANC <1500 cells/microL, and severe neutropenia as an absolute neutrophil count (ANC) <500 cells/microL. Fever in neutropenic patients is defined as a single oral temperature of >38.3°C (101°F) or a temperature of >38°C (100.4°F) sustained for >1 hour.
The absolute neutrophil count (ANC) is equal to the product of the white blood cell count (WBC) and the fraction of polymorphonuclear cells (PMNs) and band forms noted on the differential analysis:
ANC = WBC (cells/microL) x percent (PMNs + bands) ÷ 100
Etiology: Most common causes are:
-
Chemotherapy
-
Infections
-
Drugs
-
Leukemia
-
Alcoholism
-
B12/Folate deficiency
-
ARDS
-
Autoimmune diseases
-
HIV
Diagnostic Approach:
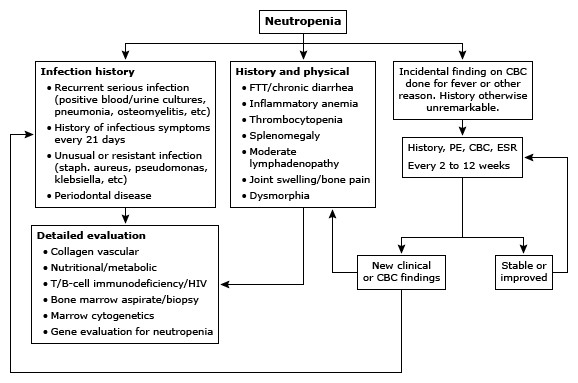
Most causes of neutropenia are benign, especially if the ANC is above 800/microL. Thus, a period of observation is indicated if the patient is asymptomatic and there are no other significant clinical features, particularly if there is a recent history of viral infection or a medication has been taken that is known to be associated with neutropenia. Examination of the oral cavity is important, since the presence of gingivitis or tooth abscess suggests the presence of symptomatic neutropenia.
Apart from blood, urine and sputum cultures, checking fungal markers from the serum, such as the Aspergillus galactomannan antigen and the beta-D-glucan assay, should also be considered in high-risk patients.
Risk Assessment:
(IDSA) has developed the following criteria for defining neutropenic patients as high-risk or low-risk when they present with a fever:
-
High-risk — High-risk febrile neutropenic patients are defined as those with any of the following characteristics:
-
ANC ≤100 cells/microL expected to last >7 days or
-
Evidence of ongoing comorbid conditions, such as hemodynamic instability, GI or oral mucositis, diarrhea, neurologic changes, intravascular catheter infection, new pulmonary infiltrate or hypoxia, chronic lung disease, hepatic insufficiency (ALT/AST >5 times normal values) or renal insufficiency.
-
-
Low-risk — Low-risk febrile neutropenic patients are expected to have a duration of neutropenia (ANC <500 cells/microL) of 7 days or fewer, and have no comorbidities or evidence of significant hepatic or renal dysfunction. They can be treated as outpatients.
-
Patients presenting with evidence of severe sepsis (sepsis syndrome with end-organ dysfunction) should be regarded as high-risk and managed with intravenously administered initial empiric antibacterial therapy and hospitalization.
Treatment:
Fever in a neutropenic patient should be considered a medical emergency. For ANC counts <500/microL, there is a significant risk of infection and fever should always be managed on an inpatient basis with parenteral antibiotics.
Gram-negative bacilli, particularly Pseudomonas aeruginosa, were the most commonly identified pathogens in neutropenic patients but there has been a shift for gram positive infections as well. Infection in severe neutropenia usually comes from the gastrointestinal tract or skin. Thus, febrile patients with neutropenia should be treated immediately, with broad-spectrum parenteral antibiotics for coverage of both Gram-positive and Gram-negative bacteria.
In general, patients with an ANC >1000/microL can be managed on an outpatient basis while those with an ANC of <500/microL and marrow aplasia may require inpatient treatment with parenteral antibiotics. Routine reverse isolation procedures are of no benefit and serve to decrease contact with medical personnel.
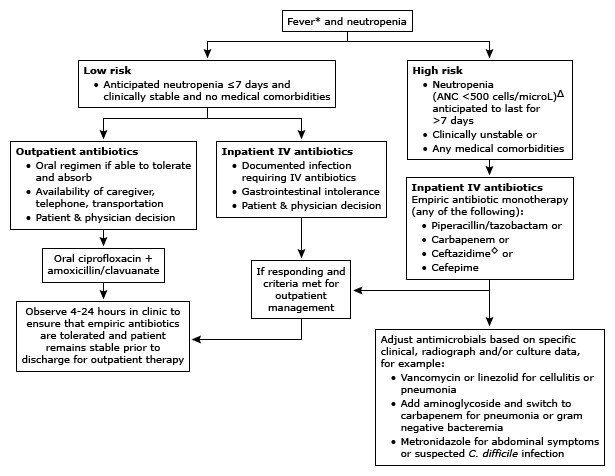
The Infectious Diseases Society of America (IDSA) recommends the following approach for the initial therapy of high-risk neutropenic patients with fever:
-
Initiation of monotherapy with an anti-pseudomonal beta-lactam agent, such as cefepime, meropenem, imipenem-cilastatin, or piperacillin-tazobactam.
-
Other antibiotics (eg, aminoglycosides, fluoroquinolones, and/or vancomycin) may be added to the initial regimen in patients with complicated presentations (eg, hypotension and/or mental status changes), or focal findings (eg, pneumonia or cellulitis).
-
Vancomycin (or other agents that target gram-positive cocci) is not recommended as a standard part of the initial regimen but should be added in certain patients, such as those with suspected catheter-related infection, skin or soft tissue infection, pneumonia, or hemodynamic instability. If vancomycin or other gram-positive coverage was started initially, it may be stopped after two to three days if there is no evidence of a gram-positive infection.
-
Modifications to the initial regimen should be considered for patients at risk for infection with antibiotic-resistant organisms, patients who are clinically unstable, and patients with positive blood cultures that are suggestive of a resistant infection.
-
Anaerobic coverage be included if there is evidence of necrotizing mucositis, sinusitis, periodontal cellulitis, perirectal cellulitis, intraabdominal infection (including neutropenic enterocolitis [typhlitis]), pelvic infection, or anaerobic bacteremia.
-
Patients who remain hemodynamically unstable after initial doses with standard agents for neutropenic fever should have their antimicrobial regimen broadened to include coverage for resistant gram-negative, gram-positive, and anaerobic bacteria and fungi
-
Empiric antifungal coverage should be considered in high-risk patients who have persistent fever after 4-7 days of a broad-spectrum antibacterial regimen and no identified source of fever.
-
Appropriate antibiotics should continue for at least the duration of neutropenia (until ANC is > 500 cells/mm3) or longer if clinically necessary
Patients receiving fluoroquinolone-based antibacterial prophylaxis should not receive a fluoroquinolone-based initial empiric antibacterial therapy
Combination therapy — Numerous combination antibiotic regimens have been studied as initial empiric therapy in neutropenic fever, but none has been shown to be clearly superior to others or to monotherapy.
The administration of recombinant granulocyte colony-stimulating factor (G-CSF, filgrastim) can correct the neutropenia and reduce infectious morbidity in infected patients with a variety of causes of severe neutropenia.
Isolation precautions:
Hand hygiene is the most effective means of preventing transmission of infection in the hospital. Standard barrier precautions should be followed for all patients, and infection-specific isolation should be used for patients with certain signs or symptoms.
Plants and dried or fresh flowers should not be allowed in the rooms of hospitalized neutropenic patients. No specific contact isolation is needed.