Chronic Obstructive Lung Disease
-
A disease state characterized by airflow limitation that is not fully reversible. It is characterized by airflow limitation that is usually progressive and associated with an enhanced chronic inflammatory response in the airways and the lung to noxious particles or gases.
-
Emphysema: anatomically defined as abnormal and permanent enlargement of the airspaces distal to the terminal bronchioles that is accompanied by destruction of the airspace walls, without obvious fibrosis.
-
Chronic bronchitis: clinically defined condition with chronic cough and phlegm for three months in two consecutive years. Small-airways disease in which small bronchioles are narrowed
-
Symptoms & Signs
- Cough, increased sputum production and dyspnea.
- Additional signs and symptoms include prolonged expiratory wheezing, decreased breath sounds, Barrel chest , large lung volumes and poor diaphragmatic excursion, use of accessory muscles of respiration , pursed lip breathing , Tripod sitting position to facilitate the actions of accessory muscles(sternocleidomastoid, scalene, and intercostal) , cyanosis visible in lips and nail beds , bitemporal wasting,
-
Traditional Clinical designation:
-
Pink puffers are patients with predominant emphysema: thin, noncyanotic at rest, and have prominent use of accessory muscles
-
Blue bloaters are patients with predominant bronchitis: heavy and cyanotic
-
- Hyperinflation flattens the diaphragm and reduces its effectiveness, making use of accessory muscles of breathing more important, and also markedly increases the work of breathing as chest wall compliance decreases.
- Cor pulmonale: Signs of overt right heart failure
Differential Diagnosis
-
CHF, Asthma, Bronchiectasis, Obliterative bronchiolitis, Pneumonia
-
Tuberculosis, Atelectasis
-
Asthma : Problems other than COPD should be suspected when hypoxemia is difficult to correct with modest levels of supplemental oxygen.
-
Lung cancer : Clubbing of the digits is not a sign of COPD.
Laboratory Tests
-
ABG's
-
Elevated hematocrit suggests chronic hypoxemia.
-
Testing for α1AT deficiency
-
Sputum Gram stain and culture (for COPD exacerbation). The value of sputum Gram stain and culture is clearer during exacerbations in patients who have risk factors for Pseudomonas infection. These risk factors include recent hospitalization (≥2 days' duration during the past 90 days), frequent administration of antibiotics (≥4 courses within the past year), severe COPD (FEV1 <50 percent of predicted), isolation of Pseudomonas aeruginosa during a previous exacerbation, colonization during a stable period, and chronic systemic glucocorticoid use.
Imaging
-
Chest radiography : obvious bullae, paucity of parenchymal markings, or hyperlucency , increased lung volumes and flattening of the diaphragm suggest hyperinflation.
-
Chest CT : definitive test for establishing the absence or presence of emphysema
Diagnostic Procedures
-
A post bronchodilator FEV1 less than 80% of predicted and FEV1/FVC less than 0.70 confirm the presence of airflow limitation that is not fully reversible.
-
Peak flow: often used as a measure of airflow limitation in asthma, but may underestimate the degree of airflow limitation in COPD
-
Pulmonary function tests/spirometry
-
Chronically reduced ratio of FEV1 to forced vital capacity (FVC)
-
In contrast to asthma, the reduced FEV1 in COPD seldom shows large responses (>30%) to inhaled bronchodilators, although improvements up to 15% are common.
-
Reduction in forced expiratory flow rates
-
Increases in residual volume
-
Increased total lung capacity (late in the disease)
-
Diffusion capacity may be decreased in patients with emphysema.
-
-
Electrocardiography may demonstrate right ventricular hypertrophy.
Classification
-
GOLD stage 0
-
Severity: at risk
-
Symptoms: chronic cough, sputum production
-
Spirometry: normal
-
-
GOLD stage I
-
Severity: mild
-
Symptoms: with or without chronic cough or sputum production
-
Spirometry: FEV1:FVC < 0.7 and FEV1 ≥ 80% predicted
-
-
GOLD stage II
-
Severity: moderate
-
Symptoms: with or without chronic cough or sputum production
-
Spirometry: FEV1:FVC < 0.7 and FEV1 50–80% predicted
-
-
GOLD stage III
-
Severity: severe
-
Symptoms: with or without chronic cough or sputum production
-
Spirometry: FEV1:FVC < 0.7 and FEV1 30–50% predicted
-
-
GOLD stage IV
-
Severity: very severe
-
Symptoms: with or without chronic cough or sputum production
-
Spirometry: FEV1:FVC < 0.7 and FEV1 < 30% predicted or FEV1 < 50% predicted with respiratory failure or signs of right heart failure
-
Classification based on pathologic type
-
Centriacinar emphysema: Type most frequently associated with cigarette smoking. Most prominent in upper lobes and superior segment of the lower lobes of the lungs
-
Panacinar emphysema: Usually observed in patients with α1AT deficiency. Most prominent in lower lobes
Treatment Approach for acute exacerbations
-
Antibiotics: COPD exacerbations can be broadly divided into infectious precipitants and non infectious precipitants. Non infectious precipitants does not need any antibiotics. Avoid routine antibiotic courses in all COPD exacerbations. GOLD guidelines recommend antibiotics only for moderately or severely ill patients with COPD exacerbations who have increased cough and sputum purulence.
-
Antivirals : check for influenxa panel, if appropriate for the season and start antivirals while the studies are pending. Rapid flu test can be falsely negative and if clinical suspicion is high, send for a PCR testing.
-
Only 3 interventions have been demonstrated to influence the natural history: Smoking cessation, oxygen therapy in chronically hypoxemic patients and lung volume reduction surgery in selected patients with emphysema
-
All other current therapies are directed at improving symptoms and decreasing frequency and severity of exacerbations.
-
β-agonists : Inhaled short-acting beta adrenergic agonists are the mainstay of therapy for an acute exacerbation of COPD because of their rapid onset of action and efficacy in producing bronchodilation. Albuterol and levabuterol are short acting and salmeterol is long acting. Terbutaline is a subcutaneous form of beta agonist. Usual dose of albuterol is 2 puffs MDI (each puff is 90 mcg) every 4-6 hrs or 2.5mg nebs every 4-6 hours. GOLD guidelines suggest that when given at appropriate doses and technique, MDI devices are equally eficacious as nebulizations. Increasing the dose to 5mg did result in significant increase in bronchodilation. Chest. 2005 Jul;128(1):48-54
-
Anticholinergic agents: Ipratropium (Atrovent) is short acting with 30-60 min onset of action and 4-h duration. Tiotropium (Spiriva) is a long acting anticholinergic drug. Other long acting anticholinergics include umeclidinium, aclidinium and glycopyrronium. In patients using tiotropium, use of atrovent may not be as beneficial because all receptors are already saturated. Usual dose of atrovent is 2 puffs MDI (each puff is 18mcg) every 4-6 hrs or 500mcg nebs every 4-6 hours.
-
Combined β-agonist/anticholinergic: Albuterol/ipratropium ( Duoneb). Addition of a β-agonist to inhaled anticholinergic therapy may provide incremental benefit (COMBIVENT Study). However, some studies showed that the combination of a beta2-agonist and ipratropium did not increase the amount of bronchodilation or FEV1 more than with beta agonists alone. (Cochrane Database Syst Rev. 2002;(4 ). Also, continuous nebulizations didn't result in any increased bronchodilation compared with intemittent dosing.
-
Inhaled glucocorticoids: Budesonide (Pulmicort) , Fluticasone (Flovent)
-
Systemic Glucocorticoids: GOLD guidelines recommend 40 mg of oral prednisolone or its equivalent for 5–14 days. GOLD guidelines as well as recent evidence shows that 5 days therapy is as efficacious as 14 day therapy ( REDUCE Trial), ( Cochrane Database Syst Rev. 2014 Dec 10 ). Also, For mild to moderate exacerbations, no difference between intravenous and oral corticosteroids. (Chest. 2007 Dec;132(6):1741-7), (JAMA. 2010 Jun 16;303(23):2359-67).
When giving IV steroids, please note that solumedrol 40mg every 6 hours is equivalent to 300mg of prednisone per day, which is a very high dose. Also, physicians very commonly increase the dose of steroids after 24 hours if the patient is still wheezing. Increasing the dose of steroids to more than 240mg of methyprednisone per day resulted in worse outcomes (Am J Respir Crit Care Med. 2014 May 1;189(9):1052-64. ). Infact some studies showed that steroids did not improve intensive care unit mortality or patient-centred outcomes in the selected subgroup of COPD patients with severe exacerbation. Eur Respir J. 2014 Mar;43(3):717-24. Also, in another study, steroids reduced the average length of hospitalization by merely 1.2 days when compared with placebo. N Engl J Med 1999; 340:1941-1947
-
Oxygen: Supplemental O2 is the only pharmacologic therapy demonstrated to decrease mortality. In resting hypoxemia (resting SaO2 < 88% or < 90% with signs of pulmonary hypertension or right heart failure), the use of O2 has been demonstrated to significantly affect mortality. Oxygen therapy is usually prescribed for patients who have arterial PO2 less than 55 mm Hg or SaO2< 88% with or without hypercapnia or who exhibit arterial PO2 of 56 to 59 mm Hg or oxygen saturation less than 89% with one or more of the following: pulmonary hypertension, evidence of cor pulmonale or edema as a result of right heart failure, or hematocrit greater than 56%.
In Long term Oxygen Treatment Trial, patients with COPD who have a resting SpO2 of more than 88%, long-term supplemental oxygen therapy did not result in longer survival than no long-term supplemental oxygen therapy, regardless of whether the patients have exercise-induced desaturation. N Engl J Med 2016; 375:1617-1627
A titrated oxygen therapy to achieve saturations of 88% to 92% is recommended in patients with an acute exacerbation of COPD to avoid hypoxemia and reduce the risk of oxygen-induced hypercapnia. Crit Care. 2012; 16(5): 323
Inability to correct hypoxemia with a relatively low FiO2 (eg, 4L/min by nasal cannula or 35% FiO2 by mask) should prompt consideration of pulmonary emboli, acute respiratory distress syndrome, pulmonary edema, or severe pneumonia as the cause of respiratory failure.
-
Other agents :
- Theophylline: Produces modest improvements in expiratory flow rates and vital capacity and a slight improvement in arterial oxygen and carbon dioxide levels in moderate to severe COPD. Intravenous aminophylline failed to show any benefit beyond that induced by inhaled bronchodilator and glucocorticoid therapy.
-
N-acetyl cysteine: Used for its mucolytic and antioxidant properties. Long-term use of oral N-acetylcysteine 600 mg twice daily can prevent exacerbations, especially in disease of moderate severity. PANTHEON Study , HIACE Study
-
Intravenous α1AT augmentation therapy for patients with severe α1AT deficiency.A randomized, controlled trial of α1AT augmentation therapy has never proved efficacious in reducing decline of pulmonary function.
-
Antibiotics: GOLD guidelines recommend antibiotic therapy for patients with a severe exacerbation requiring mechanical ventilation (noninvasive or invasive) or an exacerbation with increased sputum purulence plus either increased dyspnea or increased sputum volume. Usual antibiotics are ceftriaxone or fluoroquinolones for 3-7 days in acute exacerbations and zithromax for long term prophylaxis. Long-term suppressive or "rotating" antibiotics might be beneficial to reduce the incidence of exacerbations (N Engl J Med 2011; 365:689-698). However, long term azithromycin prophylaxis is also associated with increased cardiovascular deaths. N Engl J Med 2012; 366:1881-1890
Antibiotics during acute exacerbations showed improved outcomes for patients in ICU but had no statistically significant effect on mortality and length of hospital stay in inpatients. (Cochrane Database Syst Rev. 2012 Dec 12)
-
Annual influenza vaccine
-
Polyvalent pneumococcal vaccine is recommended.
-
Lung transplantation
-
NIPPV: Unlike asthma, COPD patients usually has a slow decline and a trial of BiPAP is worthwhile in most patients who do not require emergent intubation. It is reasonable to start with an IPAP of 10 and EPAP of 5 and titrate upwards. BiPAP with ventilators is an option and both assist control ( guaranteed ventilation) or pressure support ( patient comfort and less asynchrony) are reasonable. Patients who fail to improve on BiPAP within 1-2 hours should be promptly intubated.
It is relatively contraindicated in cardiovascular instability, impaired mental status , copious secretions or inability to clear secretions and craniofacial abnormalities or trauma precluding effective fitting of mask, high aspiration risk, on restraints. If altered mental status is due to hypercapnic encephalopathy, BiPAP for 1-2 hours is a safe and reasonable option. Chest. 2005 Mar;127(3):952-60 , Chest. 2005 Sep;128(3):1657-66
Ventilator Strategies in COPD:
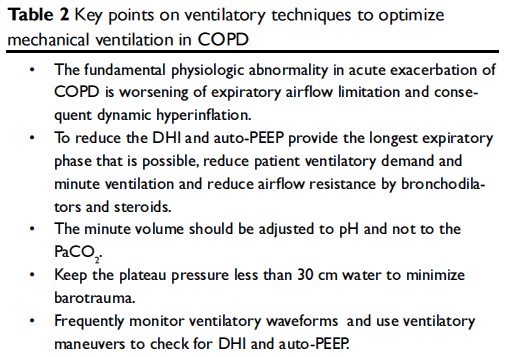
The fundamental physiologic abnormality in acute exacerbation of COPD is worsening of expiratory airflow limitation and consequent dynamic hyperinflation. These changes lead to further derangement in ventilatory mechanics, muscle function and gas exchange which may result in respiratory failure.
Dynamic hyperinflation increases the work of breathing, puts the respiratory muscles at a disadvantage, as they have to breathe at higher functional residual capacity and can cause significant cardiac dysfunction leading to worsening hypoxemia with varying degree of hypercarbia and acidosis.
Respiratory physiology
In normal subjects, in the absence of respiratory effort, the lung will come to lie at the point of the functional residual capacity (FRC). The point at which this occurs is determined by a balance between the inward elastic recoil of the lung and the equal and opposite outward recoil of the respiratory cage (mostly due to muscle tone). The intrapleural pressure (Ppl) at this point is –3 to –5 cm water. To generate a respiratory movement two factors must be overcome:
-
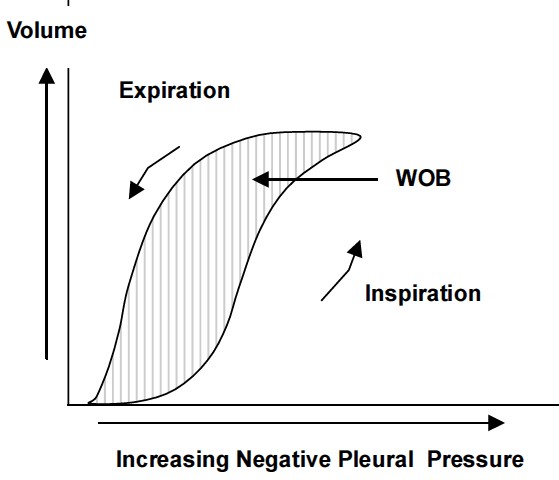
Resistance: Resistance of the airways is described as obstruction to airflow provided by the conducting airways, resulting mainly from the larger airways. Airway resistance to flow is present during both inspiration and expiration and the energy required to overcome it represents the actual work of breathing (WOB).
-
Compliance: When compliance is low, more effort is required to inflate the lungs.
Respiratory mechanics in COPD
The two primary pathophysiologic changes that contribute to the development of respiratory distress and acute respiratory failure in patients with obstructive lung disease are:
-
Increased airway resistance: Patients with COPD have increased expiratory airflow resistance. In COPD, the alveolar attachments that normally keep the smaller airways open via radial traction are lost. This leads to airway narrowing and collapse especially during expiration. In normal subjects, during passive exhalation the intrapleural pressure is negative. In COPD the intrapleural pressure may be positive during exhalation due to recruitment of expiratory muscles. As exhalation occurs, the airway resistance increases further due to compression from the surrounding positive intrapleural pressure. This causes the airway segment to collapse. Soon after the collapse occurs the intraalveolar pressure is transmitted to the collapsed segment and the airway reopens because Palv exceeds Ppl .
In acute exacerbations the already narrowed airways may be further compromised by increased secretions, mucosal swelling and peribronchial inflammation. The time constant for lung emptying is therefore prolonged and end expiratory lung volume is dynamically increased. Furthermore, during an exacerbation, patients tend to adopt a rapid shallow breathing pattern which further limits the time available for lung emptying, thus promoting greater dynamic hyperinflation (DHI) in a vicious cycle. In fact, any acute increase in ventilation (such as occurs with anxiety or transient hypoxaemia) can be associated with DHI in flow limited patients.
-
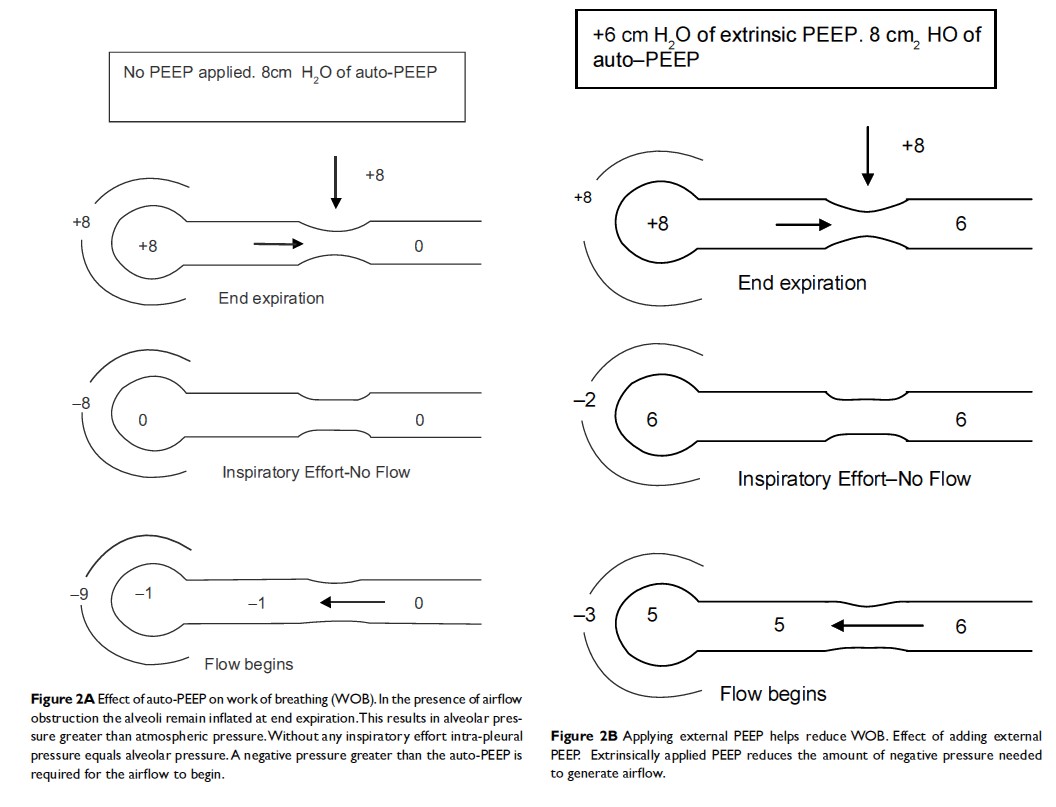
Dynamic hyperinflation: In the presence of increased expiratory airflow resistance, the time available (expiratory time) to empty the inspired volume may not be sufficient. The next inspiration may start before the completion of the expiration leading to air trapping. Thus the respiratory system is unable to return to its normal relaxation volume at the end of expiration. This results in a new resting state where the FRC is greater than the relaxation volume. This condition of air trapping is otherwise called DHI. The DHI results in positive alveolar pressure at the end of expiration also referred to as auto-PEEP (positive end expiratory pressure). Initially the auto-PEEP may be beneficial to keep the airways open and thereby reducing the airway resistance. However auto-PEEP has many disadvantages:
- Increased work of breathing (WOB): For the airflow to begin, the intrapleural pressure must fall below zero so the lung expands and the air flows in. In the presence of auto-PEEP, the intrapleural pressure generated must be more than the amount of auto-PEEP for airflow to begin which imposes a substantial inspiratory burden
- In presence of DHI, the lungs are operating at a higher than normal FRC. This causes the inspiratory muscles to operate at shorter than normal lengths. This places the respiratory muscles, in particular the diaphragm at a considerable mechanical disadvantage as they now have to operate on the flatter part of the compliance curve. As the diaphragm is lower in the chest wall during hyperinflation, its ability to descend further during inspiration is impaired.
- Excessive PEEP can compromise cardiac function in several ways. The increased intrathoracic pressure can lead to decreased venous return and decrease left ventricular compliance. Also DHI increases pulmonary capillary resistance by compressing alveolar capillaries which leads to an increase in the right ventricular after load. These changes can lead to hypotension especially soon after intubation when other factors like sedatives and hypovolemia may be coexisting.
- Regions of hyperinflated lung may compress adjacent areas of normal lung and adversely affect ventilation/ perfusion relationships
- DHI and auto-PEEP may predispose patients to barotrauma – Pneumothorax, pneumomediastinum and pneumoperitoneum may occur
- Auto PEEP and manual PEEP are not the same. Auto PEEP exists in alveoli where we don’t want any PEEP and manual PEEP is applied to alveoli where it is supposed to go.
Management
The ventilatory strategies are aimed at correcting the gas exchange abnormality, identifying and preventing DHI. The minute volume should be adjusted to pH and not to the PaCO2 to avoid over-ventilation with consequent alkali loss and reduced renal compensation.
Initial ventilator settings and the mode used is usually dependent on operator and local practices. In general low tidal volumes of 6 to 10 ml/Kg, FiO2 of 1.0, no added PEEP, respiratory of 10 to 14/minute and an inspiratory flow of 80 to 100 L/minute with square wave form are considered ideal. Ventilator-trigger sensitivity should be minimal as in the presence of auto-PEEP patient may not be able to generate enough negative pressure or flow.
In COPD patients being weaned with pressure support ventilation, appropriate setting of the cycle-off criterion is of importance to limit PEEPi and the work of breathing. Instead of cycling at 25% of peak flow, use 50% as cutoff which can decrease autoPEEP to a great extent due to increased expiratory time.
Effects of expiratory time, minute ventilation and expiratory flow rates on DHI:
The important determinants of DHI are minute ventilation, tidal volume, time for expiration, and severity of airway obstruction. Tuxen and Lane studied the various settings for minute ventilation, tidal volume and time for expiration on DHI. Minute ventilation was the most important determinant of DHI. A decrease in expiratory time (by decreasing peak flows) while keeping the minute ventilation and tidal volume constant significantly increased end expiratory volume (VEE) suggesting air trapping. A similar effect was noted with decrease of TE by increasing respiratory rate. However, if the decrease in TE was caused by an increase in tidal volume and decrease in respiratory rate while keeping constant minute ventilation only a small insignificant increase in VEE was noted. It is therefore important to recognize that a simple adjustment of Inspiratory: Expiratory (I:E) ratio is not sufficient. The adjustment to the absolute expiratory time and the minute ventilation are more important in reducing the amount of air trapping.
In general, adapting the following measures can reduce auto-PEEP:
-
Provide the longest expiratory phase that is possible. Expiratory phase can be prolonged by decreasing the respiratory rate, decreasing the tidal volume, increasing the flow rate and treating the underlying obstruction with bronchodilators. Remember that sometimes when dynamic airway collapse is present during expiration, increasing the E-time may not solve the problem. We may need to add PEEP to overcome autoPEEP.
-
Reduce patient ventilatory demand and minute ventilation.
-
Reduce airflow resistance by bronchodilators and steroids.
Adding PEEP to correct Auto PEEP
The presence of auto-PEEP acts as a threshold load for patient’s inspiratory effort. To alleviate the breathing efforts that auto-PEEP imposes on the respiratory muscles an external PEEP can be applied. It might seem that applying external PEEP is detrimental when there is already positive pressure at end expiration. This seeming paradox can be explained by analogy to a stream with waterfall. In this analogy the flow of water (airflow) is not affected until the downstream (external PEEP) rises above the critical pressure needed to constrict the airway. Above this level the external PEEP can increase upstream pressure and cause worsening DHI. The external PEEP should be kept below 75% to 85% of auto-PEEP to avoid any worsening of hyperinflation or circulatory compromise.
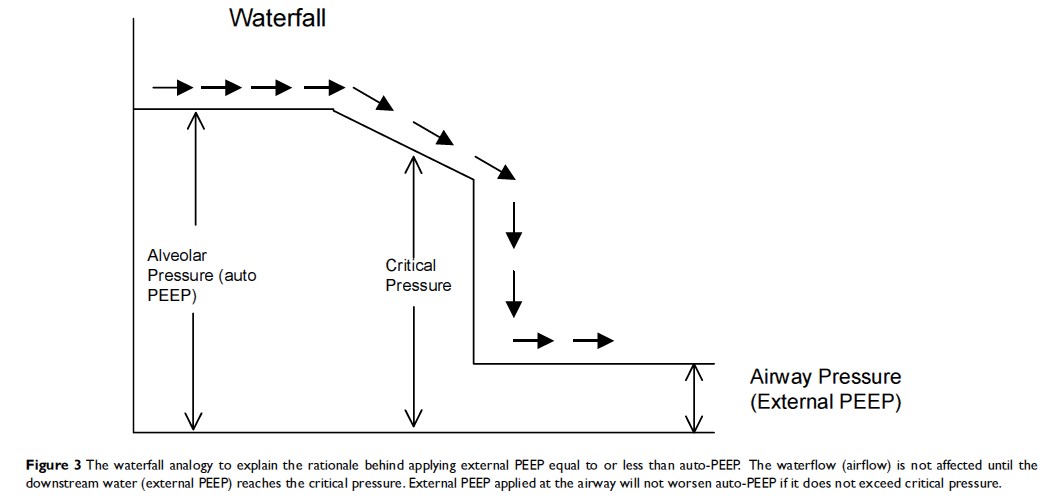
In a patient with auto-PEEP, if the ventilator is set to deliver patient initiated breaths, external PEEP can help in two ways. First, external PEEP decreases the inspiratory threshold thereby decreasing ineffective triggering and reducing the work of breathing. Second, it acts as a stent for the collapsible airways thereby increasing expiratory flow rates. ( please remember that if there is no dynamic airway collapse and if we apply PEEP, it gets transmitted directly to the alveoli and the total PEEP dramatically increases. Hence, always check the expiratory pause maneuver to see if the intrinsic PEEP increased or decreased with applying PEEP.
PEARLS
-
Inhaled medications are central to the management of chronic obstructive pulmonary disease; if a patient is not responding to therapy, the inhaler technique should be evaluated before therapy is adjusted. Most common cause of treatment failure is poor inhalation technique.
-
Do not combine short- and long-acting anticholinergic drugs. Because they both occupy the same receptors and may not be synergistic if given simultaneously.
-
The primary side effect of the inhaled anticholinergic agents used for COPD is dry mouth. Anticholinergic agents should be used with caution in patients with urinary obstruction and narrow-angle glaucoma.
-
Long-acting bronchodilators, such as long-acting β2-agonists or tiotropium, are recommended as first-line maintenance therapy when patients require regular and frequent bronchodilatory management, beginning in GOLD stage II- IV.
-
Non selective beta blockers can cause broncho constriction and it was recommended to use cardioselective betablockers like metoprolol succinate and bisoprolol. However, a small study showed that non selective betablockers are safe to use in COPD. Am J Resp Crit Car Med, Vol. 187, No. 12 (2013), pp. 1308-1314.
-
Pulmonary rehabilitation involves a combination of education, nutrition counseling, exercise training, and behavior modification techniques. The exercise component helps to improve endurance, flexibility, and strength in the upper and lower extremities, in patients with chronic lung diseases.
-
In patients with very severe COPD (stage IV), the most important sign of a severe exacerbation is sometimes a change in mental status.
-
In patients with GOLD stage II disease, maintenance treatment with one or more long-acting bronchodilators such as a long-acting β2-agonist (salmeterol or formoterol) or long acting anti-cholinergic agent is recommended, along with as-needed albuterol.
-
The long-term administration of oxygen for more than 15 hours per day to patients with chronic obstructive pulmonary disease (COPD) increases survival, and may also improve hemodynamics, hematologic characteristics, exercise capacity, lung mechanics, and mental status.
-
Regular use of inhaled corticosteroids in patients with chronic obstructive pulmonary disease (COPD) is associated with a reduction in the rate of exacerbations. Therefore, the GOLD guidelines recommend consideration of inhaled corticosteroids in patients whose lung function is less than 50% and those who have exacerbations.
-
Anticholinergic agents in COPD are especially useful when combined with short-acting or long-acting β2-agonists.
-
In moderate to severe exacerbations of chronic obstructive pulmonary disease (COPD), inhaled short-acting bronchodilators (β2-agonists and anticholinergic agents) and systemic corticosteroids, antibiotics, and supplemental oxygen are the mainstays of treatment.
-
GOLD stage III chronic obstructive pulmonary disease (COPD) defined as FEV1/FVC <70% and FEV1 30% to 50% of predicted with or without chronic symptoms (cough, sputum production). Treatment for this patient includes support for his smoking cessation, short-acting bronchodilators as needed and regular treatment with one or more long-acting bronchodilators, as well as an inhaled corticosteroid, along with pulmonary rehabilitation.
-
Routine lung expansion with incentive spirometry and deep-breathing exercises prevent postoperative pulmonary complications in patients with chronic obstructive pulmonary disease.
-
NIPPV should be initiated very early in COPD exacerbation to reduce the need for intubation, unless there is a contraindication for NIPPV. Suitable candidates for NPPV include patients with moderate to severe dyspnea, use of accessory respiratory muscles, respiration rate greater than 25/min, and pH less than 7.35 with PCO2 greater than 45 mm Hg. However, if the patient’s condition deteriorates or does not improve after 1 to 2 hours of NPPV, intubation should be considered.
-
High dose nicotine patch in combination with other anti smoking therapy like nicotine gums is the most effective therapy for smoking cessation. It works better than Bupropion or CHANTIX alone.
-
P Pulmonale-increased p wave in II, III, AVF
-
CO2 retention with oxygen therapy: Therapy with supplemental oxygen alters hypoxic pulmonary vasoconstriction and modulates the Haldane effect, resulting in changes in physiologic deadspace. Deoxygenation of the blood increases its ability to carry carbon dioxide; this property is the Haldane effect.
-
Deoxygenated hemoglobin has a higher affinity for CO2 because it is a better proton acceptor than oxygenated hemoglobin. Therefore, when hemoglobin is deoxygenated (i.e., at tissues) there is a right shift of the carbonic acid-bicarbonate buffer equation to produce H+ which in turn increases the amount of CO2 which can be carried by the blood back to the lungs to be exhaled.
-
In COPD exacerbation of unknown origin, there was a 25% prevalence of PE. Ann Intern Med. 2006;144:390-396.
-
In COPD exacerbations, if we use NIPPV, we don’t always have to use BiPAP. Using just a CPAP may be able to overcome dynamic hyperinflation and help the patient. If PCO2 is increasing with NIPPV, we commonly increase the IPAP to give more tidal volumes. However, the problem may not be the Tv but autoPEEP. By increasing the PS and thereby Tv, we may actually worsen the auto PEEP.
Check the difference between inspired and expired Tv. The difference can be due to auto PEEP or leakage. If the cause is auto PEEP, increase the EPAP rather than IPAP.
-
Beta agonists help with increased airway mucus clearance via an effect on ciliary beat frequency.
-
Hi !
why you have still 0 in the COPD classification