Liver Function Tests
-
Tests that measure detoxification or excretory functions
-
Serum bilirubin
-
Urine bilirubin
-
Blood ammonia
-
-
Serum enzymes that reflect damage to hepatocytes
-
Alanine aminotransferase (ALT)
-
Aspartate aminotransferase (AST)
-
Serum enzymes that reflect cholestasis
-
Alkaline phosphatase (AP)
-
5′-nucleotidase
-
Gamma glutamyl transpeptidase (GGT)
-
-
-
Tests that measure biosynthetic liver function
-
Serum albumin
-
Serum globulins
-
Beta globulins
-
Alpha globulins
-
Gamma globulins (immunoglobulins)
-
Coagulation factors : PT/PTT/INR
-
-
Other tests and procedures that may be necessary to make proper diagnosis of liver disease
-
Percutaneous biopsy of the liver
-
Ultrasonography
-
CT scan
-
Tests of detoxification and excretory functions
-
Serum bilirubin, Unconjugated (indirect) or Conjugated (direct). Conjugated hyperbilirubinemia almost always implies biliary tract disease, but can also be elevated in hepatocellular conditions. Elevation of unconjugated bilirubin rarely is due to liver disease.
-
Urine bilirubin. All bilirubin in urine is conjugated. In patients recovering from jaundice, the urine bilirubin clears prior to the serum bilirubin.
-
Blood ammonia. Ammonia is liberated by bacteria in the large intestine or by protein metabolism and is rapidly converted to urea in the liver. In liver disease or portosystemic shunting, the blood ammonia concentration increases. Also, significant muscle wasting contributes to hyperammonemia in advanced liver disease.
-
Aminotransferases. Intracellular enzymes involved in amino acid metabolism and released into the blood when there is damage to the liver cell membrane. AST is found in the liver, cardiac muscle, skeletal muscle, kidneys, brain, pancreas, lungs, leukocytes, and erythrocytes in decreasing order of concentration. ALT is found primarily in the liver but also in small quantities in kidney, skeletal muscle, and cardiac muscle. Increase in both ALT/AST is more consistent with liver injury than isolated increase in ALT or AST.
-
AP, 5′-nucleotidase, and GGT. Elevation reflects cholestasis.
Tests that measure biosynthetic liver function
-
Serum albumin. Synthesized exclusively by hepatocytes. Has long half-life: 18–20 days and because of this slow turnover, the serum albumin is not a good indicator of acute or mild hepatic dysfunction.
-
Serum globulins. Group of proteins made up of gamma globulins (immunoglobulins) produced by B lymphocytes and alpha and beta globulins produced primarily in hepatocytes
-
Coagulation factors. Synthesizes factors 2, 5, 7, 9, 10, 11, 12, fibrinogen, which are made exclusively in hepatocytes (except factor VIII). Serum half-lives are much shorter than albumin, ranging from 6 hours for factor VII to 5 days for fibrinogen. Because of their rapid turnover, measurement of the clotting factors is the single best acute parameter of hepatic synthetic function.
Lab tests
-
Serum bilirubin
-
Normal total serum bilirubin concentration: < 1 mg/dL
-
Up to 30%(0.3 mg/dL) of the total is direct-reacting (or conjugated) bilirubin
-
If otherwise healthy, then Gilbert syndrome; no further workup necessary
-
Isolated elevation of unconjugated bilirubin should prompt a workup for hemolysis
-
-
-
Urine bilirubin
-
Theoretically gives same information as fractionation of serum bilirubin
-
-
Blood ammonia
-
Poor correlation between the blood serum ammonia and hepatic function
-
-
Aminotransferases (ALT, AST)
-
Most helpful in recognizing acute hepatocellular diseases such as hepatitis
-
Levels >1000 U/L exclusive to extensive hepatocellular injury
-
Viral hepatitis
-
Ischemic liver injury (prolonged hypotension or acute heart failure)
-
Toxic or drug-induced liver injury
-
-
In most acute hepatocellular disorders
-
Increased ALT more prevalent than increased AST
-
-
Alcoholic liver disease
-
AST:ALT ratio > 2:1 suggestive
-
AST:ALT ratio > 3:1 highly suggestive
-
AST rarely > 300 U/L
-
-
Obstructive jaundice
-
AST and ALT usually not greatly elevated except in acute phase of biliary obstruction and can be in 1000–2000 U/L range but levels decrease quickly into a pattern of cholestasis.
-
-
-
AP, 5′-nucleotidase, and GGT
-
AP elevations > 4×normal in:
-
Cholestatic liver disorders
-
Infiltrative liver diseases (e.g., cancer and amyloidosis)
-
Bone conditions characterized by rapid bone turnover (e.g., Paget disease)
-
-
If elevated AP is only abnormal finding, or if elevation is higher than expected:
-
Measure serum 5′-nucleotidase or GGT (both rarely elevated except in liver disease)
-
-
Other conditions causing isolated elevations in AP
-
Hodgkin’s disease
-
Diabetes
-
Hyperthyroidism
-
Congestive heart failure
-
Amyloidosis
-
Inflammatory bowel disease
-
-
-
Serum albumin
-
< 3 g/dL suggests chronic liver disease. However, hypoalbuminemia can be present in nephrotic syndrome, protein losing enteropathies, malignancy, FTT, chronic infections.
-
-
Serum globulins
-
Gamma globulins are increased in chronic liver disease (e.g., chronic hepatitis, cirrhosis). Remember that gamma globulins are not manufactured in liver but by B-Lymphocytes.
-
-
Coagulation factors
-
Acute assessment of hepatic synthetic function and prognosis of acute parenchymal liver disease
-
Marked prolongation (>5 sec above control) that is not corrected by parenteral vitamin K administration indicates a poor prognostic sign in acute viral hepatitis/other acute and chronic liver diseases.
-
-
Ultrasonography
-
First test to use when liver tests suggest cholestasis
-
To look for presence of dilated intrahepatic or extrahepatic biliary tree
-
To identify gallstones
-
First test to order if Budd-Chiari syndrome is suspected
-
PEARLS:
-
2.5% of “normal” individuals will have mild elevations of a given serum liver chemistry tests. Infact, “normal physiologic” states such as pregnancy may result in markedly elevated levels of the serum alkaline phosphatase. Thus, all laboratory abnormalities must be interpreted within the clinical context of the patient.
- Viral hepatitis diagnostic markers are
Abnormal Liver tests
Reference: Gastroenterology 2002;123:1364-1366
Mild ALT and AST Elevations (<5 Times above Normal):
Chronic viral hepatitis remains one of the most common causes of abnormal liver chemistries. Other causes include Hep.B, drugs, toxins, sepsis, NASH/NAFLD, alcohol , congestive hepatopathy, rhabdomyolysis, hemochromatosis, Chronic autoimmune hepatitis, alpha one antitrypsin deficiency, celiac disease, hepatitis A/D/E and EBV/CMV viremia, HELLP syndrome and malignant infiltration of liver.
Alcoholic hepatitis is commonly associated with an AST: ALT ratio of approximately 2:1 and the AST rarely exceeds 300 IU/dL. NASH may present similarly to alcohol-related liver injury, and biopsy findings often are similar in both diseases.
Drugs that can cause hepatocellular damage include tylenol, statins, antibiotics, NSAIDS, HAART, anti tuberculosis drugs, Anti-TNF factor drugs.
Patients with suspected autoimmune hepatitis and abnormal ALT levels should have serum serologic markers measured (anti-nuclear antibodies, anti-smooth muscle antibodies, and potentially liver-kidney microsomal antibodies) and serum studies to exclude other forms of liver disease.
In patients with abnormal ALT levels of unknown origin, serum ceruloplasmin and alpha-1-antitrypsin levels can be measured to screen for Wilson’s disease and alpha-1-antitrypsin deficiency, respectively.
Reference: Gastroenterology 2002;123:1364-1366
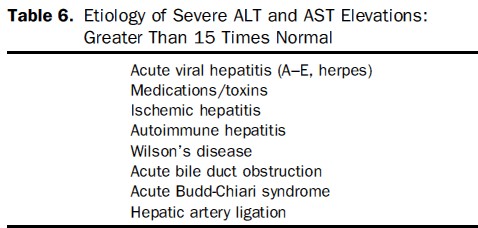
Severe ALT and AST Elevations (>15 Times above Normal):
On occasion, acute bile duct obstruction can present with marked, transient elevation in liver enzymes. Patients frequently have right upper quadrant pain and nausea, and abdominal ultrasonography may reveal biliary ductal dilatation and cholelithiasis. Liver enzymes typically decline rapidly when a stone passes out of the biliary system.
Acute vascular events such as acute Budd-Chiari syndrome, or surgical ligation or thrombosis of the hepatic artery, can present with marked elevation of liver enzymes.
Budd-Chiari frequently is characterized by the development of ascites and jaundice and is diagnosed by imaging the hepatic vein and parenchyma; it may be further confirmed by liver biopsy.
Magnitude of AST and ALT elevations — The magnitude of AST and ALT elevations vary depending on the cause of the hepatocellular injury. The following are typical AST and ALT patterns:
-
Alcoholic fatty liver disease: AST <8 times the upper limit of normal; ALT <5 times the upper limit of normal
-
Nonalcoholic fatty liver disease: AST and ALT <4 times the upper limit of normal
-
Acute viral hepatitis or toxin-related hepatitis with jaundice: AST and ALT >25 times the upper limit of normal
-
Ischemic hepatopathy (ischemic hepatitis, shock liver): AST and ALT >50 times the upper limit of normal (in addition LDH is often markedly elevated)
References:
PEARLS:
-
Only 4 conditions cause AST/ALT>3000 : Shock liver, Tylenol overdose, acute viral hepatitis and atypical viruses like HSV
-
Common ICU causes of cholestasis are gall sludge, sepsis, TPN, antibiotics like PCN.
-
Alcoholic hepatitis: Moderate elevations of the AST and ALT (typically less than 300) , elevated GGT, leukocytosis with neutrophil predominance, elevated bilirubin and INR. MELD score and discriminant factor score predict mortality. In patients with severe alcoholic hepatitis (DF ≥32), prednisone 40mg daily for 4 weeks or pentoxifylline 400mg TID for 4 weeks seems to be beneficial. STOPAH Trial , Gut. 2011 Feb;60(2):255-60
-
How can I print this?