ANTICOAGULATION IN ICU
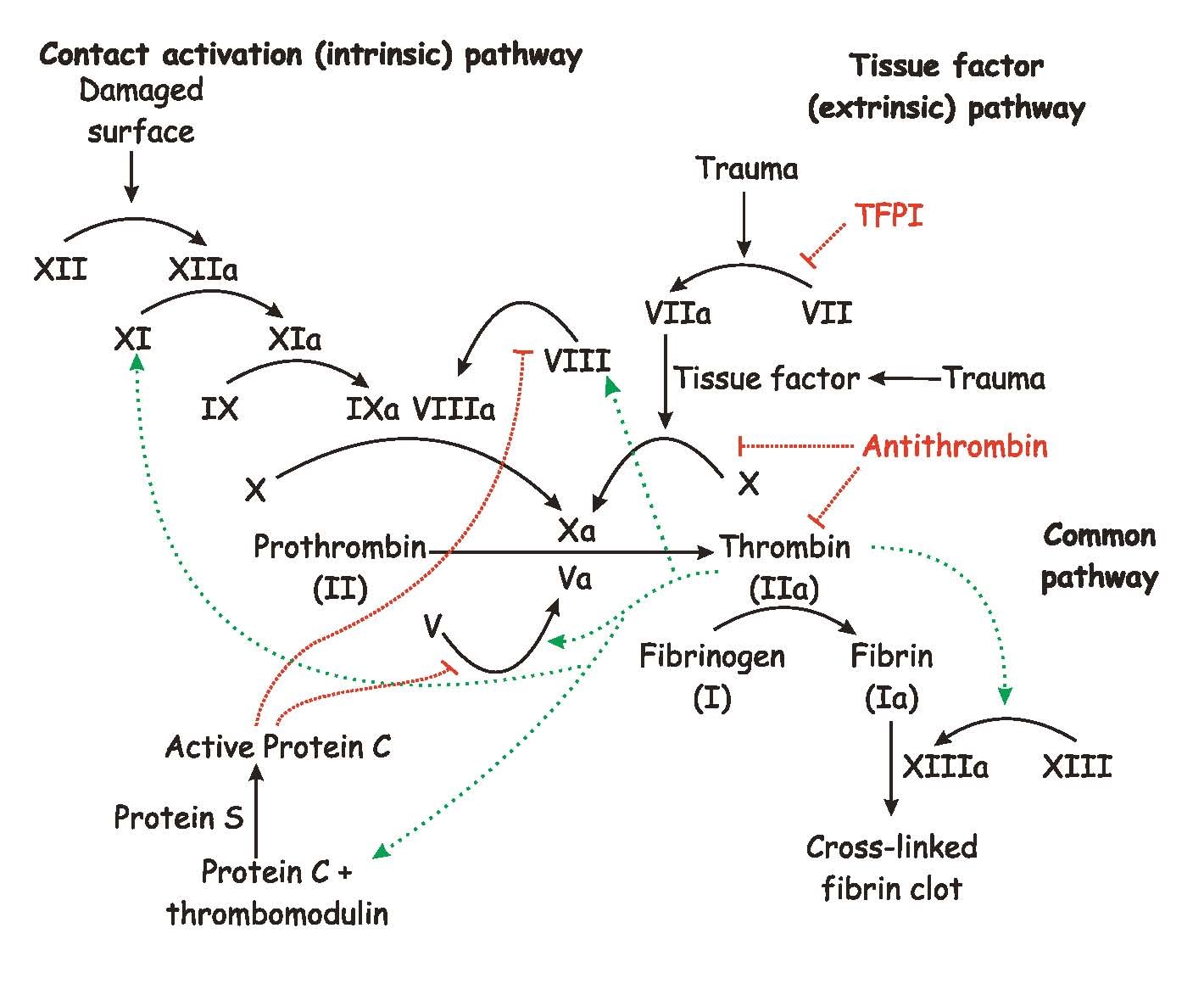
Clotting cascade:
Warfarin:
-
For patients sufficiently healthy to be treated as outpatients, we suggest initiating VKA therapy with warfarin 10 mg daily for the first 2 days followed by dosing based on INR measurements rather than starting with the estimated maintenance dose
-
For patients taking VKA therapy with consistently stable INRs, we suggest an INR testing frequency of up to 12 weeks rather than every 4 weeks
-
For patients with stable therapeutic INRs presenting with a single sub therapeutic INR, we suggest against routinely administering bridging with heparin
-
For patients taking VKAs, we suggest avoiding concomitant treatment with antiplatelet agents except in situations where benefit is known or is highly likely to be greater than harm from bleeding, such as patients with mechanical valves, patients with acute coronary syndrome, or patients with recent coronary stents or bypass surgery.
-
For patients taking VKAs with INRs between 4.5 and 10 and with no evidence of bleeding, we suggest against the routine use of vitamin K (Grade 2B). Some people may give 2.5-5 mg oral Vit.K
-
For patients taking VKAs with INR>10 and with no evidence of bleeding, we suggest that oral vitamin K be administered
-
For patients with VKA-associated major bleeding, we suggest rapid reversal of anticoagulation with four-factor prothrombin complex concentrate rather than with plasma. (Grade 2C). We suggest the additional use of vitamin K 5 to 10 mg slow IV injection rather than reversal with coagulation factors alone (Grade 2C).
-
In patients who require temporary interruption of a VKA before surgery, we recommend resuming VKAs approximately 12 to 24 h after surgery (evening of or next morning) and when there is adequate hemostasis instead of later resumption of VKAs (Grade 2C).
-
In patients with a mechanical heart valve, atrial fibrillation, or VTE at high risk for thromboembolism, we suggest bridging anticoagulation instead of no bridging during interruption of VKA therapy (Grade 2C). In patients with a mechanical heart valve, atrial fibrillation, or VTE at low risk for thromboembolism, we suggest no bridging instead of bridging anticoagulation during interruption of VKA therapy (Grade 2C).
-
In patients who require dental surgery or minor skin surgeries or cataract surgery and are receiving VKA therapy, we suggest continuing VKAs around the time of the surgery instead of other strategies (Grade 2C).
-
Antidote: Vit.K 5-10mg IV; full effect occurs only after 24 hrs but usually some effect seen in 6-12 hours.
-
IV Vit.K works quicker than oral at 6 hour mark but probably the same at the end of 24 hours.
-
Coumadin induced necrosis: stop Coumadin immediately and start heparin drip.
Heparin:
UFH binds to anti-thrombin and thereby accelerating inactivation of activated clotting factors IIa (thrombin), IXa, Xa, XIa and XIIa, subsequently halting coagulation. LMWH also binds to Antithrombin, but due to smaller size, it preferentially inhibits factor Xa.
Half life of UFH is 90 mins and wears off in 2-4 hours. Half life of LMWH is 6 hrs and wears off in 12 hours.
Enoxaparin: 1 mg/kg every 12 hours or 1.5 mg/kg daily
Dalteparin: 200 IU/kg daily or 150IU/Kg BID (Maximum of 18000 units per day)
UFH: Initial rate of a bolus 80 units/kg followed by 18 units/kg/hr for VTE; bolus 70 units/kg followed by 15 units/kg/hr for cardiac or stroke patients)
-
For outpatients with VTE treated with SC UFH, we suggest weight-adjusted dosing (first dose 333 units/kg, then 250 units/kg) without monitoring rather than fixed or weight adjusted dosing with monitoring (Grade 2C) .
-
In patients who are receiving bridging anticoagulation with therapeutic-dose LMWH, we suggest administering the last preoperative dose of LMWH approximately 24 h before surgery instead of 12 h before surgery (Grade 2C) .
-
In patients who are receiving bridging anticoagulation with therapeutic-dose LMWH and are undergoing high-bleeding-risk surgery, we suggest resuming therapeutic-dose LMWH 48 to 72 h after surgery instead of resuming LMWH within 24 h after surgery (Grade 2C) .
-
Antidote: Protamine sulphate – 1mg of Protamine neutralizes approximately 100 units of UFH; Use only the last 3 hours when considering the amount of heparin administered to patient, due to the short half‐life of UFH. Maximal dose is 50mg. There will be a full reversal with UFH and 60-80% reversal with LMWH but no reversal with fondaparinux. Recheck PTT or factor Xa level and re-dose, if needed. Administer protamine IV with maximum infusion rate of 5 mg/min to prevent hypotension and bradycardia. Onset of reversal effect is seen 5 minutes after administration but duration of reversal activity is approximately 2 hours.
-
Protamine: The dosing of protamine for LMWHs is significantly less complicated than UFH. Dosing recommendations are 1 mg of protamine for every 100 anti-Xa units of LMWH (Enoxaparin 1mg = 100 anti-Xa units) administered over the previous 8 hours with a maximum protamine dose of 50 mg. If it has been greater than 8 hours since the last LMWH dose, the dose of protamine decreases to 0.5 mg for every 100 anti-Xa units of LMWH. Reversal is 60-80% for LMWH and 100% for UFH.
Fondaparinux
It is an indirect factor Xa inhibitor. Elimination half life is 17-21 hrs and drug effect lasts for 2-4 days after stopping. It is excreted mainly by kidneys.
-
Daily dose: <50 kg: 5 mg. 50-100 kg: 7.5 mg. >100 kg: 10 mg.
-
For patients with VTE and body weight over 100 kg, we suggest that the treatment dose of fondaparinux be increased from the usual 7.5 mg to 10 mg daily SC
-
It doesn’t affect PTT or INR. In high risk patients, monitor factor Xa levels
-
There is no specific antidote. FFP/PCC can be considered.
-
Used for DVT/PE, ACS, dvt prophylaxis but contraindicated if CrCl<30.
Argatroban, Bivalirudin, Lepirudin:
-
These are intravenous direct thrombin inhibitor.
-
Monitoring by PTT values. But, argatroban also increases PT/INR and clotting time.
-
Argatroban is metabolized by liver and needs dose adjustment in liver failure.
-
Bivalirudin is metabolized by enzymatic breakdown and 20% by kidneys.
-
They are approved for ACS and NSTEMI/STEMI with PCI and HIT.
-
There is no specific reversal agent or antidote. Due to the short half-life of these agents, management of hemorrhagic complications is primarily supportive and interruption of treatment will be sufficient to reverse the anticoagulant effect. For refractory bleeding, PCC complex or FFP can be considered even though there is no proven benefit.
-
Argatroban wears off in 4 hours and bivalirudin wears off in 2 hours.
Dabigatran:
Dosing: CrCl >30 ml/min: 150 mg orally, twice daily
CrCl 15-30 ml/min: 75 mg orally, twice daily
-
It is an oral direct thrombin inhibitor. It prolongs PTT and thrombin time but they don’t reflect the degree of activity of pradaxa. I.e. those tests are poor markers of dabigatran overdose.
-
Dabigatran etexilate, the prodrug, is converted in the liver to the active compound dabigatran, which then binds directly to thrombin with high affinity and specificity.
-
Dabigatran has rapid onset of action within a half-life of approximately 12 to 14 hours and is excreted in urine in an unchanged form.
-
There is a new antidote for Dabigatran ( Praxbind) related bleeding and it is the only oral anticoagulant which is dialyzable.
-
It is approved for non –valvular A.fib and prevention of VTE.
-
Not recommended for those with CrCl<30.
-
Higher incidence of thrombotic events in patients with mechanical heart valves. Hence, the trial was stopped in valvular heart disease patients with A. Fib.
Rivaroxaban, Apixiban:
-
These are oral factor Xa inhibitors and has rapid onset of action. Both are highly protein bound and not dialyzable. Excreted by liver and kidneys.
-
Can affect PTT/INR in a variable manner.
-
Usually reversed with 4 factor prothrombin complex. Monitor PT/INR, PTT and Factor Xa levels for reversal efficacy.
-
Approved for non valvular A. Fib and treatment of VTE.
-
Usual dose for rivaroxaban is 15mg BID for 3 weeks followed by 20mg daily and for apixiban is 5mg BID. Not recommended for those with CrCl<30.
Aspirin/Plavix:
-
In patients who are receiving ASA and require coronary artery bypass graft (CABG) surgery, we suggest continuing ASA around the time of surgery instead of stopping ASA 7 to 10 days before surgery (Grade 2C) . In patients who are receiving dual antiplatelet drug therapy and require CABG surgery, we suggest continuing ASA around the time of surgery and stopping clopidogrel/prasugrel 5 days before surgery instead of continuing dual antiplatelet therapy around the time of surgery
-
In patients with a coronary stent who are receiving dual antiplatelet therapy and require surgery, we recommend deferring surgery for at least 6 weeks after placement of a bare-metal stent and for at least 6 months after placement of a drug-eluting stent instead of undertaking surgery within these time periods (Grade 1C) . In patients who require surgery within 6 weeks of placement of a bare-metal stent or within 6 months of placement of a drug-eluting stent, we suggest continuing dual antiplatelet therapy around the time of surgery instead of stopping dual antiplatelet therapy 7 to 10 days before surgery (Grade 2C).
-
Aspirin, clopidogrel, Ticlopidine, and prasugrel inhibit platelet function for lifetime of platelet. Inhibition takes 7-10 days to resolve as new platelets are generated.
-
Ticagrelor (Brilinta)/NSAIDS/Dipyridamole are reversible inhibitors, so platelet function normalizes after drug clearance.
-
ASA or plavix overdose can be treated with platelets and DDAVP.
DVT Prophylaxis
-
For acutely ill hospitalized medical patients at increased risk of thrombosis, we recommend thromboprophylaxis with LMWH, low-dose unfractionated heparin (UH) bid, UH tid, or fondaparinux.
-
For acutely ill hospitalized medical patients at low risk of thrombosis, we recommend against the use of pharmacologic prophylaxis or mechanical prophylaxis
-
For general and abdominal-pelvic surgery patients at high risk for VTE in whom both LMWH and unfractionated heparin are contraindicated or unavailable and who are not at high risk for major bleeding complications, we suggest low-dose aspirin (Grade 2C) , fondaparinux (Grade 2C) , or mechanical prophylaxis, preferably with IPC (Grade 2C) , over no prophylaxis.
-
For craniotomy and spinal surgery patients at very high risk for VTE (eg, those undergoing craniotomy for malignant disease), we suggest adding pharmacologic prophylaxis to mechanical prophylaxis once adequate hemostasis is established and the risk of bleeding decreases (Grade 2C) .
-
In patients undergoing THA or TKA, we recommend DVT prophylaxis for a minimum of 10 to 14 days: low-molecular-weight heparin (LMWH), fondaparinux, apixaban, dabigatran, rivaroxaban, low-dose unfractionated heparin (LDUH), adjusted-dose VKA, aspirin (all Grade 1B), or an intermittent pneumatic compression device (IPCD) (Grade 1C).
-
In patients undergoing Hip fracture surgery, we recommend DVT prophylaxis for a minimum of 10 to 14 days: LMWH, fondaparinux, LDUH, adjusted-dose VKA, aspirin (all Grade 1B), or an IPCD (Grade 1C).
-
For patients undergoing major orthopedic surgery (THA, TKA, HFS) and receiving LMWH as thromboprophylaxis, we recommend starting either 12 h or more preoperatively or 12 h or more postoperatively rather than within 4 h or less preoperatively or 4 h or less postoperatively.
-
For patients undergoing major orthopedic surgery, we suggest extending thromboprophylaxis in the outpatient period for up to 35 days from the day of surgery rather than for only 10 to 14 days (Grade 2B).
-
In patients with an intermediate clinical suspicion of acute VTE, we suggest treatment with parenteral anticoagulants compared with no treatment if the results of diagnostic tests are expected to be delayed for more than 4 h (Grade 2C). However, in patients with high suspicion, we prefer to empirically start treatment. (Grade 2C)
DVT Treatment:
-
In patients with proximal DVT or pulmonary embolism (PE), atleast 3 months of anticoagulant therapy is recommended (Grade 1B).
-
In patients with a second unprovoked VTE or active cancer, extended anticoagulant therapy (no scheduled stop date) is recommended (Grade 1B).
-
In patients with DVT/PE but without any cancer, newer anticoagulants like dabigatran, rivaroxaban, apixaban, or edoxaban are recommended over coumadin therapy (Grade 2B). In there is any evidence of cancer, LMWH is recommended over other anticoagulants.
-
If DVT is provoked by surgery or a transient risk factor, 3 months of anticogulation is recommended over extended therapy (Grade 1B).
-
In patients with acute isolated “distal” DVT of the leg and without severe symptoms or risk factors for extension, we suggest serial imaging of the deep veins for 2 weeks over initial anticoagulation (Grade 2C) . In patients with acute isolated distal DVT of the leg who are managed with serial imaging, we recommend no anticoagulation if the thrombus does not extend (Grade 1B) ; we suggest anticoagulation if the thrombus extends even if it remains confined to the distal veins (Grade 2C) ;
-
In patients with acute isolated distal DVT of the leg and severe symptoms or risk factors for extension , we suggest initial anticoagulation over serial imaging of the deep veins (Grade 2C) .
-
In patients with acute DVT of the leg, we recommend early initiation of VKA and continuation of parenteral anticoagulation for a minimum of 5 days and until the international normalized ratio (INR) is 2.0 or above for at least 24 h.
-
In patients with acute proximal DVT of the leg, we suggest anticoagulant therapy alone over catheter-directed Thrombolysis or systemic thrombolysis or thrombectomy (Grade 2C) .
-
In patients with acute DVT of the leg, we recommend against the use of an IVC filter in addition to anticoagulants (Grade 1B).
-
In patients with acute proximal DVT of the leg and contraindication to anticoagulation, we recommend the use of an IVC filter (Grade 1B) .
-
In patients with acute DVT of the leg, we suggest early ambulation over initial bed rest (Grade 2C).
-
In patients with an isolated distal DVT of the leg provoked by surgery or by a nonsurgical transient risk factor, we suggest treatment with anticoagulation for 3 months.
-
In patients with superficial vein thrombosis of the lower limb of at least 5 cm in length, we suggest the use of a prophylactic dose of fondaparinux or LMWH for 45 days over no anticoagulation (Grade 2B).
-
For upper extremity DVT involving axillary or more proximal veins, anticoagulation is recommended for 3 months.
-
In most patients with UE DVT that is associated with a central venous catheter, we suggest that the catheter not be removed if it is functional and there is an ongoing need for the catheter (Grade 2C).
-
In patients with symptomatic splanchnic vein thrombosis (portal, mesenteric, and/or splenic vein thromboses), we recommend anticoagulation over no anticoagulation (Grade 1B). In patients with incidentally detected splanchnic vein thrombosis (portal, mesenteric, and/or splenic vein thromboses), we suggest no anticoagulation over anticoagulation (Grade 2C).
-
In patients with symptomatic or incidental hepatic vein thrombosis, we suggest anticoagulation over no anticoagulation. (Grade 2C)
-
In malignancy associated DVT, prefer twice daily LMWH instead of once a day regimen.
-
For recurrent DVT inspite of being on anticoagulants, switching to a different anticoagulant is reasonable.
PE treatment:
-
In patients with subsegmental PE (no involvement of more proximal pulmonary arteries) with no proximal DVT in the legs and have a low risk for recurrent VTE, clinical surveillance by serial ultrasound is recommended over anticoagulation (Grade 2C)
-
In patients with acute PE, when a thrombolytic agent is used, we suggest short infusion times (eg, a 2-h infusion) over prolonged infusion times (eg, a 24-h infusion) (Grade 2C) .
-
In patients with acute PE when a thrombolytic agent is used, systemic thrombolysis through a peripheral vein is recommended over a catheter directed thrombolysis (Grade 2C).
-
In patients with acute PE associated with hypotension and who have contraindications to thrombolysis or failed thrombolysis, or shock that is likely to cause death before systemic thrombolysis can take effect (eg, within hours), if appropriate expertise and resources are available, we suggest catheter-assisted thrombus removal over no such intervention (Grade 2C) .
-
In patients with acute PE who are treated with anticoagulants, we recommend against the use of an IVC filter (Grade 1B).
Prosthetic Valves:
-
In patients with aortic bio prosthetic valves, who are in sinus rhythm and have no other indication for VKA therapy, we suggest aspirin (50-100 mg/d) over VKA therapy (Grade 2C) .
-
In patients with a bioprosthetic valve in the mitral position, we suggest VKA therapy (target INR, 2.5; range, 2.0-3.0) over no VKA therapy for the first 3 months after valve insertion (Grade 2C).
-
In patients with a mechanical mitral valve, we suggest VKA therapy with a target of INR 2.5-3.5
Stroke:
-
In patients with acute ischemic stroke in whom treatment can be initiated within 4.5 h of symptom onset, we recommend IV r-tPA
-
In patients with acute ischemic stroke or TIA, we recommend early (within 48 h) aspirin therapy with an initial dose of 160 to 325 mg over therapeutic parenteral anticoagulation (Grade 1A).
-
In patients with acute primary Intracerebral hemorrhage and restricted mobility, we suggest prophylactic-dose SC heparin (UFH or LMWH) started between days 2 and 4 or intermittent pneumatic compression devices (Grade 2C).
-
In patients with a history of non cardioembolic ischemic stroke or TIA, we recommend long-term treatment with aspirin (75-100 mg once daily), clopidogrel (75 mg once daily), aspirin/ extended-release dipyridamole (25 mg/200 mg bid), or Cilostazol (100 mg bid).
-
In patients with a history of ischemic stroke or TIA and atrial fibrillation, including paroxysmal AF, we suggest oral anticoagulation with dabigatran 150 mg bid over adjusted-dose VKA therapy (target range, 2.0-3.0) (Grade 2B).
-
In patients with a history of ischemic stroke or TIA and atrial fibrillation, including paroxysmal AF, who are unsuitable for or choose not to take an oral anticoagulant, we recommend combination therapy with aspirin and clopidogrel over aspirin (Grade 1B).
-
In patients with cerebral venous sinus thrombosis, we suggest anticoagulation over no anticoagulant therapy during the acute and chronic phases (Grade 2C).
Peripheral Vascular Disease:
-
For persons with asymptomatic peripheral arterial disease (PAD), we suggest aspirin 75 to 100 mg daily over no aspirin therapy (Grade 2B) .
-
For patients with intermittent claudication refractory to exercise therapy (and smoking cessation), we suggest the use of cilostazol in addition to previously recommended antithrombotic therapies (aspirin 75-100 mg daily or clopidogrel 75 mg daily)
-
In patients with acute limb ischemia due to arterial emboli or thrombosis, we suggest immediate systemic anticoagulation with unfractionated heparin and reperfusion therapy.
-
For patients undergoing peripheral artery percutaneous transluminal angioplasty with or without stenting or patients undergoing peripheral artery bypass grafting, we recommend long term aspirin (75-100 mg/day) or clopidogrel (75 mg/day) (Grade 1A).
-
For patients with asymptomatic carotid stenosis, we suggest aspirin 75 to 100 mg daily over no aspirin therapy (Grade 2B) .
-
In patients with symptomatic carotid stenosis (including recent carotid endarterectomy), we recommend long-term antiplatelet therapy with clopidogrel (75 mg once daily) or aggrenox or aspirin (75-100 mg once daily).
-
Aspirin, clopidogrel, Ticlopidine, and prasugrel inhibit platelet function for lifetime of platelet. Inhibition takes 7-10 days to resolve as new platelets are generated. Ticagrelor is a reversible inhibitor, so platelet function normalizes after drug clearance.
PEARLS:
-
Time it takes for full therapeutic effect for Vit. K(24 hours), FFP(6 hours) and PCC(3-4 minutes)
-
PCC contain coagulation factors 2, 7,9,10 as well as proteins C and S.
-
Platelet transfusion may not completely restore platelet function in patients under clopidogrel, but it is efficient for patients under aspirin. Same thing for DDAVP.
-